Chu said:
And thanks Gaby. That's very clear. My bad, it's actually IgGs they test (title of the thread modified accordingly). But I still don't know, is it a reliable test, or is it something that changes regularly, and not worthy of testing, really? Because from what I understand, these antibodies may not have been there to begin with, but one develops these intolerances with time. So does that mean that they can also "go away", together with the intolerance, if one stops eating the culprit foods for a while, or do we always keep these antibodies? Sorry for being dense here...
And what is the relationship between these intolerances and epigenetics? Can these antibodies generate gene mutations? (I'm asking that because in the case of Hydradenits Suppurativa, for example, I remember reading something about an experiment where some genetic mutations were discovered with time apart from the gene which is supposed to be mutated already from birth, and is one of the alleged (they're not sure) culprits.
IgG is much better, but it has a half life of about one month or perhaps a bit more, I'm not sure. Definitely not years. It also has at least three subclasses: IgG1, IgG2, IgG3. Perhaps this is why the test is so expensive.
As I understand it, if the diet has been clean, it is not worth testing antibodies for food sensitivity. Even though some memory may lie within the antibody, the activity should be silenced if no food culprits are eaten. In other words, the antibody is not triggered even though it holds a memory of a food sensitivity.
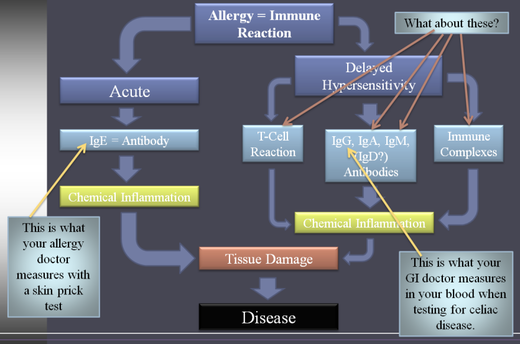
The immune system is related with gene mutations. As I understand it, it would be something like this:
Epigenetic factor exposure in early childhood or womb ------> epigenetic changes ----> gene mutates ------> altered gene triggers the immune system in a unique "pathological" way in response to a perceived assault from the environment in order to defend the body.
Let me quote a summary I wrote awhile ago, see if it helps clarify (or not :/):
There is a genetic predisposition where HLA-DQ genes located on chromosome 6 makes you vulnerable to gluten intolerance. HLA stands for the human leukocyte antigen (HLA) system, which is also known as the major histocompatibility complex (MHC). The important thing to know about this system is that it contains a large number of genes related to the function of the immune system.
This brings the subject of the fixed genetic myth... We now understand that it is really the epigenetic factors, the ones that are beyond the control of the gene, that are determining how DNA will be interpreted, translated and expressed. It is the epigenetic factors that are determining which genes will turn on and which ones will shut-off. And it is the diet and our environment along with its tons of pollutants the ones influencing the epigenetic factors. That is, our food sources and our environmental exposure affect our DNA and its expression. As Sayer Ji (2010) writes,
[N]utritional deficiencies of selenium, zinc, riboflavin, vitamin E, etc. in the womb or early in life, may “trigger” the faulty expression or folding patterns of the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) gene in Cystic Fibrosis which might otherwise have avoided epigenetic activation. This would explain why it is possible to live into one’s late seventies with this condition, as was the case for Katherine Shores (1925-2004). The implications of these findings are rather extraordinary: epigenetic and not genetic factors are primary in determining disease outcome. Even if we exclude the possibility of reversing certain monogenic diseases, the basic lesson from the post-Genomic era is that we can’t blame our DNA for causing disease. Rather, it may have more to do with what we choose to expose our DNA to.
In view of this information, Sayer argues how celiac disease is an expression of a natural, protective response to the ingestion of something that the human body was not designed to consume. He adds:
If we view celiac disease not as an unhealthy response to a healthy food, but as a healthy response to an unhealthy food, classical CD symptoms like diarrhea may make more sense. Diarrhea can be the body’s way to reduce the duration of exposure to a toxin or pathogen, and villous atrophy can be the body’s way of preventing the absorption and hence, the systemic effects of chronic exposure to wheat.
Sayer's article can be found here: http://www.greenmedinfo.com/page/dark-side-wheat-new-perspectives-celiac-disease-wheat-intolerance-sayer-ji
Perhaps Hydradenits Suppurativa is an acute way to detoxify the glands or body from a toxin or food sensitivity. What triggers the immune response or antibodies is the big question.
Some antibodies turn against other antibodies in certain autoimmune conditions. An example is what is called "rheumatoid factor" measured in lab tests where IgM turns against IgG. Under normal circumstances, antibodies is something our bodies naturally produce and they do not turn against us. What epigenetic factors are turning them to misfire or create disease?
The immune system is very complex and some admit there are many more responses researched and not published in textbooks, hence, not measured in lab tests.
The HLA system and its relation with both genes and immune system is very interesting. Possibly there is more to it than we currently know... or that I can remember.