Over the past couple of months, I have been doing a lot of research on the effectiveness of the clinical application of thyroid hormones for a variety of disease-states (which are traditionally not thought of as being induced by thyroid inadequacy). I recently came across the blogger named "Valtsu" who's work is very interesting and seems to synthesise a lot of this information in an understandable way. Below is a fascinating article with heaps of research which supports the notion that heart disease (amongst other things) may stem from undetected thyroid hormone dysfunction. This may be something worthy of consideration for members on the forum who either have pre-existing cardiovascular pathology, or simply present with precursor biomarkers like high cholesterol etc.
Link to the article with references and appendices is here.
"One of my recurring objects of thought has been the slowness with which raw knowledge is assimilated. For example, I have been thinking about Broda Barnes’s work on the prevention of heart disease with thyroid extract. He did solve much of ‘the riddle of heart attacks,’ but recent statements by the Heart Association show that the dominant forces in the health business haven’t learned anything at all from his work, which he began 50 years ago. His work is clearly presented, not hard to understand, and it is scientifically so sound that no one challenges it, at least not on the scientific level. It is ignored, rejected by people who choose not to be bothered to read it. How many people have died from heart disease, since his work first became available? (And how many more from cancer, tuberculosis, and other diseases he showed occur mainly among hypothyroid people?)"- Raymond F. Peat
1. Introduction
This review addresses the hypothesis that thyroid insufficiency could be a significant cause of the heart disease and that the traditional thyroid medication (desiccated thyroid) could therefore be a logical strategy for an effective prophylaxis for heart disease. There is a considerable amount of studies carried out on this subject that aren’t very well-known despite their remarkable results.
In addition to describing these studies conducted mostly in the middle of the 20th century, some parts regarding diagnosis, causes, and treatment of hypothyroidism are included.
2. Regarding the current CVD treatments
In the last few decades, a large part of the discussion related to heart disease (CVD) has been about cholesterol levels. The modern theories of heart disease often focus on the effect of LDL cholesterol in the genesis of atheroma plaques (in the intima part of blood vessels).
This is also the reason why low-fat or low-saturated fat diets are recommended for the prevention of heart disease. Saturated fat is supposed to cause CVD by increasing the serum concentration of LDL cholesterol. It’s also the reason why a large amount of the western human population uses cholesterol-lowering drugs, statins.
These two methods, however, haven’t proved very effective. Especially, if we look at the recent meta-analyses compiling evidence from a large amount of fat-modification trials, they don’t support the view that saturated fat is an important cause of CVD. (Hooper 2011, Ramsden 2010, Skeaff&Miller 2009)
Statins, on the other hand, have proved effective. Meta-analysis published in 2012 revealed that in the context of secondary prevention, statins can decrease total mortality by 20 per cent in men, though no significant benefit was seen in women. Also, the Cochrane review published in 2011 showed that in primary prevention, statins can decrease total mortality by 16 per cent, and heart attacks by a few dozen per cent. (Gutierrez et al. 2012, Taylor et al. 2011)
(My note: scrap this information about statins. They are quite simply the devil in a pill)
These results are quite good, but since we want to maximize the effectiveness of medications and even statins do leave a majority of people vulnerable to CVD deaths, it's always good to think about alternative ways to minimize the harms of cardiovascular disease.
3. Desiccated thyroid and CVD, part I: William B. Kountz
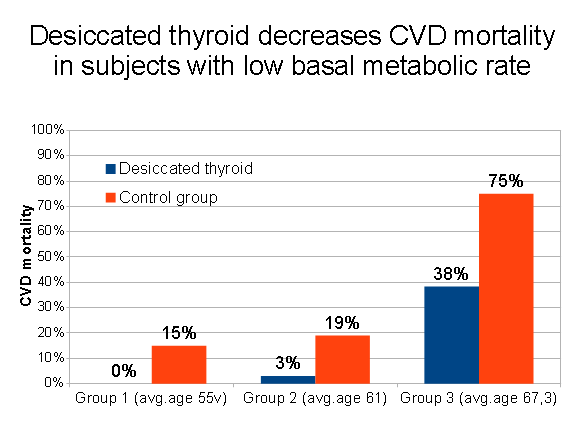
In 1951, physician William B. Kountz published his monograph Thyroid function and its possible role in vascular degeneration, in which he introduced his 5-year study with 268 subjects.
As study subjects, Kountz had specifically chosen people with low basal metabolic rate (BMR; on average, 10 to 18 percent below normal). For the intervention groups he prescribed desiccated thyroid to raise their metabolic rate to the normal level. The control group did not get thyroid. Both groups got some B vitamins as well.
There were three intervention groups plus their corresponding control groups. Group 1 consisted of middle-aged businessmen, Group 2 consisted of middle-aged office workers, and Group 3 consisted of elderly infirmary patients.
The study results were promising. The rates of heart attacks were 85, 76 and 44 per cent lower in the intervention groups (group 1, 2 and 3). The reductions in mortality were similar, and are shown below.
4. Desiccated thyroid and CVD, part II: James C. Wren
Two decades after Kountz’s research, physician James Wren conducted two studies which gave additional support to Kountz’s results.
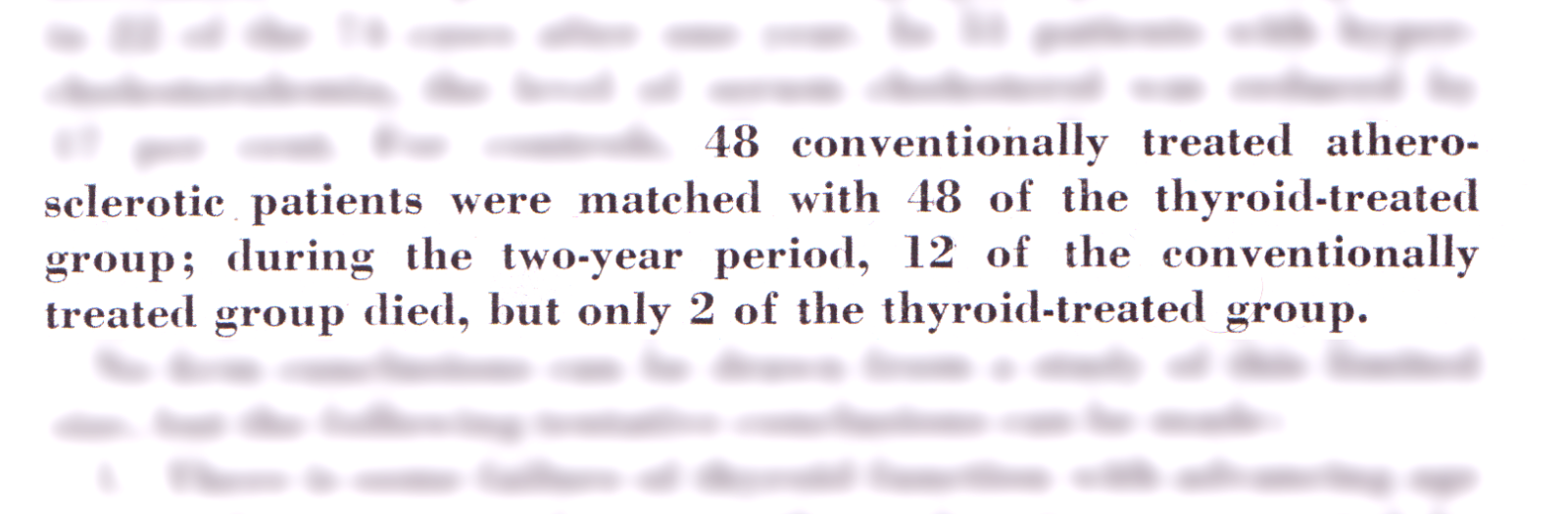
The first study, Thyroid function and coronary atherosclerosis, was published in 1968. During the two years, 74 CVD patients were given desiccated thyroid plus some vitamins. Forty-six controls were matched for the same number of intervention subjects.
The results were positive. The thyroid treatment decreased subjects’ pains, improved their ECGs and lowered their cholesterol levels 17 per cent on average. 95 per cent of the subjects reported subjective benefit from the treatment. The difference in the mortality rates between the intervention and control group was six-fold (2 vs 12).
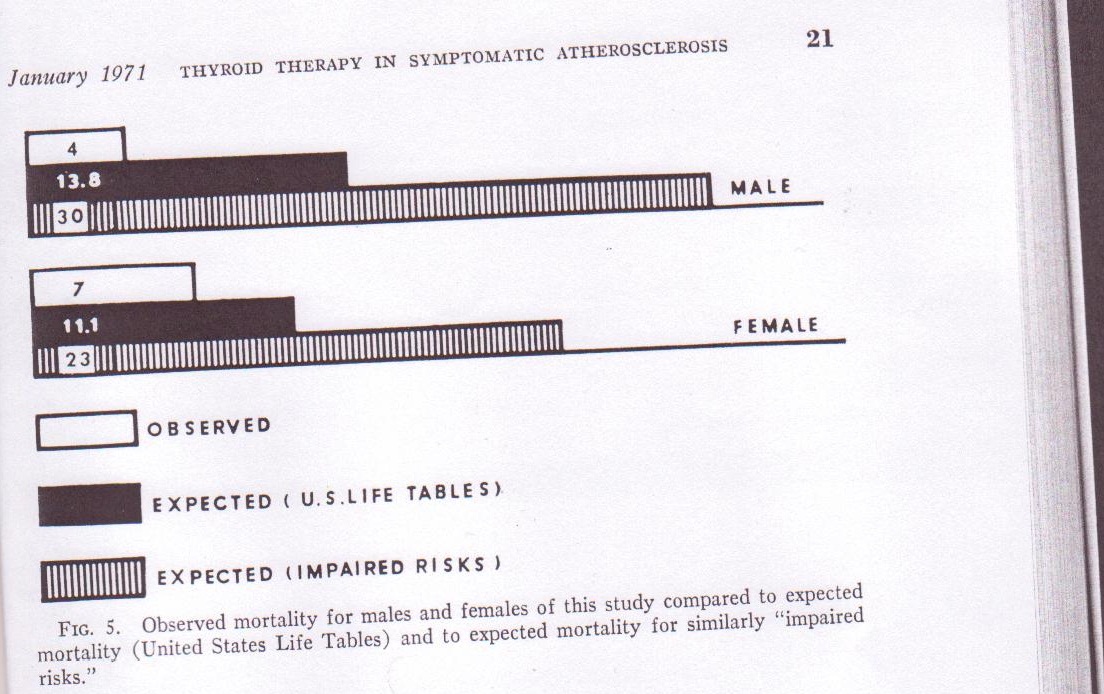
The results of a second and a little bit larger study, Symptomatic atherosclerosis: prevention or modification by treatment with desiccated thyroid were published 1971.
In this five-year study there were 347 CVD patients (1/3 of them were symptomatic), all of which were put on desiccated thyroid medication even though only 9 per cent of them had hypothyroidism based on the blood tests.
There was no control group, but during the five years of study there were half as many deaths as the statistics would have predicted for the people of the same age. When a rough adjustment for the risk factors (heart disease, hypertension etc) was made, it was clear that the subjects had a fortunate survival rate. Their mortality was only one fifth of the expected number (11 vs. 53).
5. Desiccated thyroid and CVD, part III: Broda Barnes
Physician Broda Otto Barnes‘ dissertation, published in 1932, was related to the function of the thyroglobulin protein. In the beginning of his medical practice, he noticed that many of his patients had symptoms that were similar to mild hypothyroidism. After noticing this, he began prescribing desiccated thyroid to a large part of his patients.
Barnes didn’t diagnose hypothyroidism based on his patients’ blood tests or basal metabolism (BMR), but instead he claimed that basal temperature is a more accurate marker of thyroid hormone function and health. His essay on that subject, Basal temperature versus basal metabolism, was published in 1942 in The Journal of the American Medical Association. In that article, Barnes wrote that he told his patients to measure their axillary temperature immediately after waking up. Temperature lower than 36.5 celcius (97.8F) was an important indicator of hypothyroidism and thus, a need for a prescription of desiccated thyroid.
Thirty years later, in 1973, Barnes published some of his patient data in his article On the genesis of atherosclerosis. The occurrence of CVD in his 1500+ patients was 94% lower than Framingham statistics would have predicted. This is a remarkable result considering that Barnes didn’t advocate his patients to quit smoking or change their other habits.
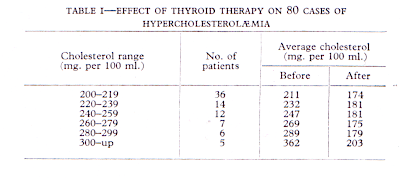
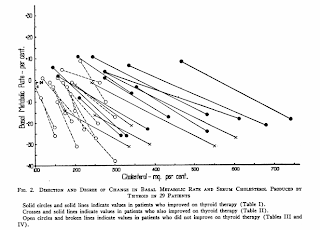
I think it’s wise to mention one of Barnes’ other papers too, Prophylaxis of ischaemic heart-disease by thyroid therapy (1959), published in Lancet. The paper shows that thyroid treatment lowers high cholesterol levels very reliably.
For his study, Barnes chose 80 persons who had high cholesterol (>200mg/dl). Usually the cholesterol levels fell to the range of 170-200mg/dl or 4.4-5.2 mmol/l after the patients had been on their thyroid medication for a sufficient duration.
(My note: Thyroid hormone is required for the conversion of cholesterol to Pregnenolone (the ultimate precursor for all sex hormones). This means that someone presenting with high cholesterol may in-fact have low thyroid hormone with NORMAL TSH + T3 + T4. Blood thyroid tests only measure blood thyroid levels, and do NOT measure tissue thyroid availability nor cell utilisation. Therefore, we see that thyroid tests may be useless in some contexts.)
6. Desiccated thyroid and CVD, part IV: Mark Starr, Lerman&White, Russek, Strisower, Moses&Danowski and Eaton
Physician Mark Starr (who has written a book Hypothyroidism Type 2: The Epidemic) has treated his patients according to Broda Barnes’ recommendations. In his book, he mentions that despite having treated over 1600 patients, only two have had a heart attack.
“I have treated over 1,600 patients during my 14 years of private practice and only two have had a heart attack while under my care.” - Mark Starr, MD
In 1946, Jacob Lerman and Paul D. White described how of 27 young CVD patients, 21 had BMR less than 10 per cent below normal. Desiccated thyroid raised their BMR and lowered their cholesterol levels. According to Lerman ja White, they couldn’t make any clear conclusions from their observations, but in all except two patients with angina pectoris a little amount of thyroid extract decreased or cured the pain. And the patients without previous angina pectoris symptoms didn’t suffer any adverse effects from thyroid extract either. (J Clin Invest 1946; 25:914)
In 1959, Henry I. Russek wrote in Circulation the following:
“To access the effects of thyroid therapy in patients with coronary artery disease, this hormone, or an identical placebo, was administered to 58 clinically proven cases of angina pectoris. All patients studied were determined to be euthyroid by appropriate tests (BMR, PBI, and cholesterol). [...]
Although all patients have been taking maximum doses [180mg] of thyroid extract for 6 to 15 months, no complications from therapy have been observed. Exercise-electrocardiographic tests have not demonstrated diminution in exercise tolerance and, in fact, have shown improved response in 6 patients. Forty-six patients reported subjective benefit as evidenced by an improved sense of well being, greater motivation, alertness and increased exercise tolerance. These observations are not only contrary to the traditional view that thyroid extract is dangerous in the presence of coronary heart disease, but also establish a rationale for its use in selected euthyroid patients with this disorder.” (Circulation 20: 761, 1959)
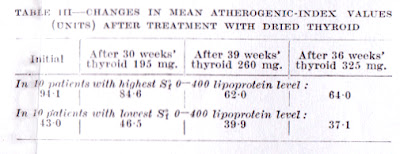
In 1957, Strisower et. reported about a two-year-study, in which subjects were given desiccated thyroid (up to 325mg) to lower their cholesterol levels (baseline 216mg/dl). The medication was most useful for those who had the highest initial cholesterol levels. Based on this finding, the group summarized: “The large falls in atherogenic-index values for patients with high initial atherogenic index values suggest that dried thyroid is worthy of consideration as a prophylactic agent against coronary heart-disease.” (Strisower et al. 1957)
In 1958, Moses ja Danowski wrote about their 10-month trial in which desiccated thyroid (150-180mg) was given for elderly people institutionalized for custodial care. The report says:
“While maintaining a normal protein bound iodine level, statistically significant decreases in total cholesterol and [beta]-lipoprotein cholesterol were found in the great majority of subjects. [...] the data indicate that even in subjects euthyroid by the usual indices, a thyroid deficit exerting considerable effect on the cholesterol-lipoprotein partition may be present.” (Circulation 1958; 18: 761)
In 1954, C.D. Eaton, a physician from Detroit published an scientific paper about the remarkably high incidence of hypothyroid symptoms in diabetics. Eaton noted that the patients often responded positively to desiccated thyroid and that they also had less of the vascular complications associated with diabetes. (Eaton 1954)
7. Other human and animal studies regarding the link between CVD and thyroid hormones
Now we have gone through the clinical data regarding prevention of heart disease with thyroid. Next, we are going to look at some indirect evidence from other kinds of studies.
1) Clinical hypothyroidism causes heart disease, and thyroxine prevents this effect
In clinical hypothyroidism, LDL levels do increase and LDL also oxidizes much faster than usually (lag time 29min), but thyroxine (T4) restores LDL levels and oxidation rate to normal (lag time 77min). (Diekman et al. 1998) This phenomena is at least partially related to the physiological fact that triiodothyronine (T3) increases hepatic LDL receptor activity, which causes LDL to stay less time in the blood because of the increased uptake*. Serum free T3 is also inversely associated with heart disease. (Lopez et al. 2007, Bakker et al. 1998, Scarabottolo et al. 1986, Ertas et al. 2012)
Clinically and subclinically hypothyroid people have increased intima-media thickness (IMT), and thyroxine resolves this problem. (Nagasaki et al. 2003, Duman et al. 2007, Monzani et al. 2004, Adrees et al. 2009, Cakal et al. 2009)
Treating subclinical hypothyroidism with thyroxine reduced the total mortality of patients (age less than 70) 64% compared to the control group. The reduction in the total mortality was mainly due to reduced cardiovascular and cancer mortality. (Razvi et al. 2012)
On one study, subclinical hypothyroidism was quite strongly correlated with an increased risk of myocardial infarction in elderly women (OR 2.3). In other studies the link seems to be a little bit weaker. (Hak et al. 2000, Rodondi et al. 2010)
Clinical (and some studies, subclinical) hypothyroidism is associated with increased levels of homocysteine and Lp(a) and increased plasma viscosity. Increased levels of fibrinogen have also been found in subclinical hypothyroidism, but T4 didn’t lower it. (Kutluturk et al. 2013, Adrees et al. 2009, Caraccio et al. 2002, Hussein et al. 1999, Catargi et al. 1999, Erdem et al. 2008, Cakal et al. 2007).
2) Very often, people with heart disease have also thyroid (gland) problems
István Gáspár studied patients who died from atherosclerosis (n=55). Seventy-one per cent of them had abnormally small thyroid glands. Twenty-four patients also had signs of thyroid inflammation, fibrosis and other kinds of thyroid degeneration. (Gaspar 1968)
Gordon J. Azar noticed that in his group of 73 heart attack survivors, approximately half of the subjects had marginal or submarginal thyroid function according to the protein-bound iodine PBI test. (Azar 1965)
Unto Uotila’s group, here in Finland in the ’50s, noticed that 58% of men and 50% of women dying of CVD had goiter, while amongst people dying because of other cause, 28% of men and 22% of women had goiter. (Uotila et al. 1958)
Dean and Fowler found that women with coronary artery disease have exaggerated TSH response to TRH-stimulation. (Dean&Fowler 1985)
3) Higher TSH levels are correlated with raised cholesterol and heart disease even within normal range
The HUNT study included more than 25,000 Norwegians. The women with TSH in the range of 1.5-2.4, had 41 per cent higher CVD mortality the women whose TSH was in the range of 0.5-1.4. TSH of 2.5-3.5 was correlated with 69 per cent increased heart mortality. For men, the trend was not statistically significant. (Asvold et al. 2008)
It has also been shown that higher TSH is associated with less favourable serum lipids and higher blood pressure even in the normal TSH range. (Asvold et al. 2007, Boggio et al. 2014) We also know from the 30′s that cholesterol levels higher than 7mmol/L is strongly correlated with hypothyroidism, and usually thyroid extract lowers the cholesterol levels sufficiently. (Barnes 1959, Hurxthal 1934, Gildea et al. 1939, Michalopoulou et al. 1998 etc…)
http://2.bp.blogspot.com/-lYiUmejo7Yg/UQVqF_2pszI/AAAAAAAABGg/K2Z1sRTNRjU/s1600/hurxthal1934.jpg
The cholesterol levels increase to the left, correlating with hypothyroid symptoms (Clinical Myxedema) (Hurxthal, 1934)
In hypothyroid patients, the cholesterol levels go down when basal metabolic rate goes up.(Gildea, 1939)
4) Lower free T4, even within reference ranges, is associated with poorer cardiovascular health
It has been noted in a couple of studies that even in clinically euthyroid people, lower FT4 levels are correlated with increased intima-media thickness, calcium scores and risk of hypertension. (Kim et al. 2012a, 2012b, Takamura et al. 2009, Dullaart et al. 2007, Gumieniak et al. 2004)
5) The herbivore cholesterol feeding studies
Pathologist Nikolai Anichkov is considered a very important person in the history of cholesterol theory. He showed that “without cholesterol there’s no atherosclerosis.” In 1912, he fed rabbits with cholesterol in vegetable oil medium, and because of this, rabbits developed atherosclerosis. In 1933 Anichkow stated that this rabbits’ atherosclerosis is similar to human atherosclerosis.
In the same year, Kenneth B. Turner and I.B. Friedland published their own studies on the same topic. Turner noticed that cholesterol feeding raised rabbits’ cholesterol levels to very high levels (13.45mmol/L), and feeding thyroid extract prevented this (4.60mmol/L). Iodine had a similar effect, but thyroxine prevented the rise in cholesterol levels only slightly. Friedland noticed the same thing: thyroid extract prevented cholesterol-induced rise in the serum cholesterol and atherosclerosis. (Turner 1933, Friedland 1933, Hoption Cann 2006)
In the beginning of ’60s, Bernick et al. studied the differences between cholesterol metabolisms of herbivores compared to omnivores. They noticed that the thyroid glands of omnivores expanded (hyperplasia) after cholesterol feeding, possibly due to increased thyroid hormone requirements in liver.** The thyroid glands of the herbivores became smaller (hypoplasia), and they developed atherosclerotic lesions. (Bernick et al. 1962)
In 1964, L.V. Malysheva noticed that feeding rabbits with cholesterol lowered their metabolic rate even in the important tissues such as liver and brain, and in the long term during the development of atherosclerosis this effect became even larger. The magnitude of this decrease in metabolism has been compared to the post-thyroidectomy decrease in metabolism. (Malysheva 1964, Duntas&Wartofsky 2007)
6) Hypertension
Hypertension is an important risk factor of CVD. Desiccated thyroid seems to be a quite potent medication for hypertension.
In 1952, Pericles Menof published his treatment results based on the data of 334 patients in South African Medical Journal. He had begun to treat essential hypertension with sole thyroid. Based on his 4-year experience, he reported that 69 per cent of his hypertensive patients benefited from the treatment, and that the lack of results in some patients can be explained by their renal hypertension which couldn’t be cured by thyroid. (Menof 1952)
Fifteen years later Menof had the same thoughts regarding hypertension and thyroid, and in the conclusions of his paper he stated that “relative thyroid insufficiency is the basic factor in the causation of essential hypertension”. (Menof 1967) Later, he also reported the cholesterol-lowering effect of thyroid extract based on his experience with over 100 patients. He also thought that benefits of thyroid hormones might be related to their antagonistic effect to hyperlipidemic effects of adrenaline and hypertensive effects of noradrenaline. (Menof 1973)
"If we are prepared to accept this view, then we must also accept the conclusion that in the timeo use of the thyroid hormone we have the solution to the Western world's most pressing medical problem - the prevention and control of atherosclerotic arterial disease."- Pericles Menof (1973)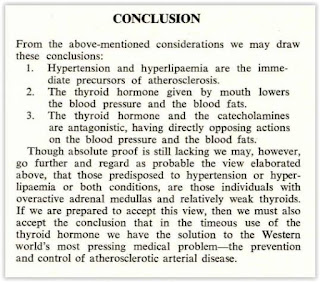
In 1971, Broda Barnes wrote in the Federation Proceedings, that during 20+ years and 1000+ patients, only twelve patients developed hypertension and of 127 hypertensive patients, 102 benefited from thyroid. He also stated that the reductions in blood pressure happen quite slowly and might take up to three years. (Fed Proc. Vol 31, Issue 2, s. A214)
Moreover, Fang and Reyes have also studied the usage of desiccated thyroid in the treatment of hypertension, but I haven’t managed to obtain the full text. According to a secondary source, “they were the first to report a coincident fall in the pulse rate in the majority of the cases successfully treated (68%).” (Fang&Reyes 1953, Menof 1967)
Fang also reported beneficial effects on total cholesterol: "Fourteen cases with hypercholesterolemia of various etiologies were treated with thyroid extract at the dosage of 2-6 grains daily for periods varying from 4 weeks to 16 months. Lowering of the serum cholesterol was noted in all cases. Elevation of the same was noted after the suspension of the therapy. There were no side effects noted". (Fang&Serrano 1960)
7) Thyroid hormone analogs
"Today, statins are used as the first treatment choice to lower plasma total and LDL cholesterol levels, but high-risk patients still experience further events of CHD. Thus, there is a need for novel pharmacological strategies. Preclinical and clinical studies using selective [thyroid hormone] analogs are promising and suggest TRβ1 as a potential target for treatment of dyslipidemia."
- (Pramfalk et al. 2011)
Various molecules that have similar properties to thyroid hormones are a relatively hot topic in the medical research, and there have been studies especially for treating high cholesterol levels and heart failure (Baxter&Webb 2009, Cioffi et al. 2010)
Thyroid hormone analogue eprotirome (KB2115) has been shown to decrease and improve cholesterol levels very effectivele. Some animal studies have shown it to cause cartilage damage, so the research regarding this drug was temporarily stopped. However, a more recent 3-month human study showed a beneficial effect on cholesterol levels with no evidence of adverse effects. (Berkenstam et al. 2008, Ladenson et al. 2010, Lin et al. 2012, Angelin et al. 2015)
Another thyroid analogue, sobetirome (GC-1), is provisionally a promising drug, but it hasn’t been tested on humans yet. (Grover et al. 2004, Baxter et al. 2004, Johansson et al. 2005, Venditti et al. 2009, Tancevski et al. 2011, Lin et al. 2012, Mitchell 2013)
Furthermore, neither of thyroid analogues MB07811 and KB-141 have been tested on humans, but in short-term animal studies, the results have been encouraging. (Erion et al. 2007, Cable et al. 2009, Ito et al. 2009 and Grover et al. 2005, Bryzgalova et al. 2008)
A very new drug, MGL-3196, has been Phase I tested with humans in a 2-week study, and the results showed a very beneficial effect on the cholesterol levels. (Taub et al. 2013)
8. Regarding the diagnostics: Is the incidence of hypothyroidism underestimated?
One important thing to remember now is that none of the physicians who saw reduced heart disease in their patients using desiccated thyroid (Kountz, Wren, Barnes, Starr) diagnosed their patients according to the typical guidelines, but instead they based their diagnoses on other markers such as basal metabolic rate, basal metabolism and heart disease.
Here in Finland, it’s generally accepted that no more than half a million Finns suffer from thyroid symptoms. That would equal nine percent of the Finnish population.
However, some doctors such as Broda Barnes have stated that there are probably a lot more people who would benefit from thyroid treatment. According to Barnes, in 1976 approximately 40% of Americans had symptoms of hypothyroidism. In 1989, Jacques Hertoghe estimated that in Belgium, up to 80 per cent of the population suffered from hypothyroid symptoms.
(My note: I would expect this figure to have risen significantly since then. Consider the fact that PUFA, bromine, xenoestrogens, and other toxins have become more abundant than ever in the last 30 or so years. These factors all inhibit thyroid function.)
In common language, “hypothyroidism” refers mainly to primary hypothyroidism, in which the thyroid gland doesn’t produce thyroid hormones normally, and because of that TSH levels are high and T4 and/or T3 levels are low. The most common reason for primary hypothyroidism is Hashimoto’s thyroiditis. It's quite common especially in women.
However, in addition to actual hypothyroidism, some groups seem to suffer from a low metabolism and various symptoms which seem to be alleviated or cured by thyroid extract.
Two examples of this are polycystic ovary syndrome (PCOS) and fibromyalgia. In one study it was found that women with PCOS had remarkably low basal metabolic rates, yet in another study it was shown that the majority of these women had normal serum levels of thyroid hormones. In one study, they also got impressive results with thyroxine: "Of the 22 patients with mild hypothyroidism, 10 had polycystic ovaries before thyroxine therapy. In all these patients, the polycystic appearance of the ovaries regressed after euthyroidism was achieved for at least 3 months." (Georgopoulos et al. 2009, Benetti-Pinto et al. 2013, Muderris et al. 2011)
Fibromyalgia, as a disease, shares many similarities with hypothyroidism. In fibromyalgia, both metabolic rate and basal temperature are reduced as in hypothyroidism. Lowe has reported that even “euthyroid” people (with normal serum levels of thyroid hormones) get good results with T3 medication. According to Broda Barnes, more common ailments such as migraine, recurring infections, acne, menstrual irregularities, and mental disturbances often go hand in hand with low basal metabolic rate and are often cured when the patient’s metabolic rate goes up with thyroid medication. (Lowe&Yellin 2008, Lowe et al. 2006, Barnes 1947, Barnes 1949, Foster 1939, Litzenberg 1937 etc…)
I think that some mechanism other than low thyroid hormone concentration in serum could cause hypothyroid symptoms. The mechanism is probably related to function of receptors and target tissues. Maybe many people have underlying metabolic problems caused by deficiencies, infections or other things, which inhibit thyroid hormone function and aerobic metabolism on the tissue level.
It has been observed that people with similar serum levels of thyroid hormones can have very different thyroid hormone levels in tissues. (Peeters 2005, check Fig 1 and Fig 2) Deiodinases can activate or inactivate thyroid hormones inside the cell, and therefore serum levels of thyroid hormones “do not faithfully reflect thyroid hormone signaling in cells.” (Bianco 2013, Gereben et al. 2008) Lowered thyroid hormone activity within the cell could be the reason why some people need TSH-suppressive doses of thyroid hormones in order to feel healthy. (Fraser et al. 1986)
9. Various thyroid medications (T4, T3, T4+T3 and desiccated thyroid)
In the above studies examining the possibility prophylaxis of heart disease with thyroid hormone, natural desiccated thyroid was used instead of synthetic hormones.
As a medication, NDT became popular in the ’30s, but after the sixties the synthetic hormones have replaced them almost completely. So nowadays most hypothyroid patients receive T4 monotherapy. Sometimes but still quite rarely patients are treated by synthetic combination therapy (T4+T3), sole triiodothyronine (T3) or desiccated thyroid (NDT; Armour Thyroid being the most popular trademark).
Can it be said that one of these medications is better than the others?
The question isn’t an easy one. In some studies combination therapy or NDT has brought clear benefits to the patients(+), but in many studies no benefit was found. However, in several studies the patients preferred the combination therapy to T4 therapy(#), even if there were no differences in symptom scores. In some studies, the addition of T3 was associated with the improvement of cholesterol levels(&). In one old study, the combination therapy led to worse results than T4 therapy(-). (Nygaard et al. 2009(+,#), Bunevicius et al. 1999(+,#), Bunevicius et al. 2002(+,#), Cooke et al. 1992(+), Solter&Solter 2012, Fadeyev et al. 2010(&), Celi et al. 2011(&), Hoang et al. 2013(#), Appelhof et al. 2005(#,&), Escobar-Morreale et al. 2005(#), Rodriguez et al. 2005(#), Slawik et al. 2007(+), Clyde et al. 2003, Walsh et al. 2003, Sawka et al. 2003, Regalbuto et al. 2007, Valizadeh et al. 2009, Smith et al. 1970(-), Pepper&Casanova-Romero 2014(#))
On the other hand, Baisier et al. compared T4 to NDT treatment and in their study, the desiccated thyroid seemed to outdo the synthetic treatment in every possible way. The authors also state that urine free T3 is a more worthy marker than the typical blood tests. NDT-treated patients had much higher urine free T3 than those who received synthetic treatment. (Baisier et al. 2001, pdf)
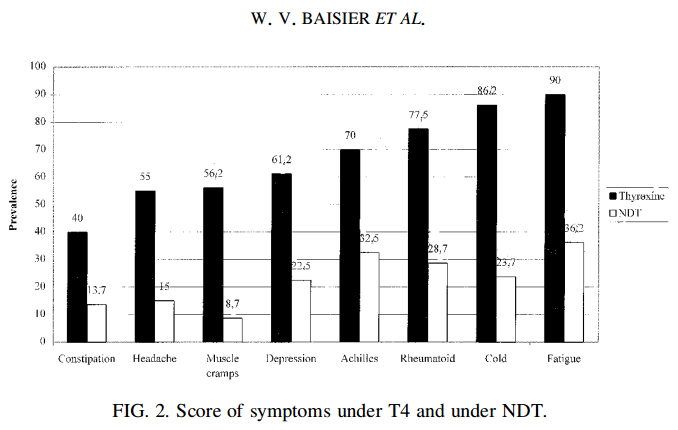
In this study, patients felt much better on desiccated thyroid medication (Baisier 2001)
In a way it’s quite contradictory that in some studies, combination treatment is associated with better results while in other studies, no difference has been noted. Lowe (2006) has stated that the differing results are not due to chance, but because of differing methods between studies: combination treatments (incl. T3) could often be more effective than T4 treatment, but the effectiveness can’t usually be seen in typical replacement therapy in which the main goal is to normalize TSH. Instead, the dose should be adjusted by other markers such as symptoms or basal metabolic rate — in the most successful studies the results seem to have been achieved by such treatments. When the dose of thyroid hormone replacement is adjusted according to symptoms, sometimes sufficient treatment will suppress thyrotropin (TSH) to very low or even undetectable levels. (Lowe 2006, Fraser et al. 1986, Cooper-Kazaz et al. 2007)
One reason why TSH-suppressive doses appear helpful, could be the fact that TSH by itself seems to be able to cause inflammation. The progression of Hashimoto's thyroiditis to hypothyroidism can sometimes be prevented with thyroxine, and one explanation for this could be the fact that the thyroid-stimulating effect of TSH might also cause or aggravate inflammation of the tissue. (Dardano 2007, Gavin et al. 2008, Padberg et al. 2001, Takasu et al. 1992, Aksoy et al. 2005, Romaldini et al. 1996, Schumm-Draeger et al. 1996, Reinhardt et al. 1988, Braga et al. 2001, Gagnon et al. 2014, Ericson et al. 1972)
There are a couple of differences between NDT and levothyroxine (synthetic T4) that aren’t discussed very often. In desiccated thyroid, the hormones are not free. Instead, they seem to be bound to thyroglobulin. Desiccated thyroid also seems to contain some other biologically active molecules such as T2 and calcitonin, both of which seem to have some potentially useful effects on animals. (Moreno et al. 2011, Mollica et al. 2009, Lombardi et al. 2009, Lanni et al. 2005, Lanni et al. 1998, Lanni et al. 1992 & Feigh et al. 2013, Robert et al. 1982)
Some studies have also been published on T3 monotherapy. Lowe reported that supraphysiological doses of T3 is an effective and safe treatment for fibromyalgia, even in euthyroid subjects. Celi et al. have reported that using T3 treatment for hypothyroidism, instead of T4, improves the body weight and cholesterol levels of the subjects. In some studies, T3 monotherapy has been useful for asthma, depression, and some types of bipolar disorder. However, many studies have also been unable to demonstrate any benefit for depression. (Lowe et al. 1996, Lowe et al. 1997, Lowe et al. 1998, Celi et al. 2011, adbel Khalek et al. 1991, Kelly&Lieberman 2009, Posternak et al. 2008, Iosifescu et al. 2005, Goodwin et al. 1982, Cooper-Kazaz et al. 2007)
In one large study with approximately one thousand subjects, dextro form of thyroxine (T4) was tried for atherosclerosis prophylaxis. However, the medication increased the total mortality a little bit. Nowadays, levothyroxine has completely replaced this less potent form of T4. (The Coronary Drug Project 1972, Barnes 1972)
There is also a huge amount of discussion about various types of thyroid therapy on the Internet (social media). I’m quite impressed about the numerous anecdotes of better results with NDT (or combination) therapy compared to T4 monotherapy. Many of these patients also report that their medication suppresses their TSH to about zero.
10. Possible causes of thyroid deficiency / lowered metabolic rate
The function of thyroid hormones is related to a large amount of metabolic processes, so it wouldn’t be very illogical to think that in some people, the inadequate metabolic rate (or thyroid function) could be related to their diet or lifestyle. Below I demonstrate some of the possible associations between diet, lifestyle, thyroid hormone function and CVD.
Nutritional deficiencies - Iodine deficiency is obviously the most well-known cause of hypothyroidism and goiter. Here in Finland, a large percentage of the population suffered from iodine deficiency goiter in the ’50s. However, salt and some other foods have been fortified with iodine since those times and therefore the deficiency is quite rare nowadays. (Lamberg 1986, Lamberg 2003) (My note: we know this not to be the case)
Selenium is another trace mineral which is closely related to the thyroid function. In cholesterol-fed rabbits, the combination of selenium and vitamin E gives better protection from atherosclerosis than vitamin E alone. (Schwenke&Behr 1998) In Finland, soils were quite depleted of selenium until the beginning of 1980s. (Arthur 2003, Hoption Cann 2006)
I have been thinking that the additions of iodine and selenium to the Finnish food supply might have been one of the main contributors to the decline in coronary heart disease during the North Karelia project. The common view is that the project decreased CVD mortality by advocating people to eat less saturated fat (SFA) and to start exercising.
However, I think it’s quite probable that decreased SFA intake didn’t affect the mortality nearly as much as the changes in iodine and selenium consumption. Paavo Roine’s research group stated in 1958, that while there was higher CVD mortality in the eastern Finland, North Karelia in particular, fat consumption didn’t differ in the east, compared to the western Finland. However, iodine intake was a little bit lower in the eastern Fnland.*** So maybe we shouldn’t blame fat, but iodine deficiency instead. (Roine et al. 1958)
Another mineral related to thyroid hormone function and atherosclerosis is copper. Copper deficiency seems to cause cardiovascular disease and low dietary intake correlates with metabolic syndrome, which again is negatively correlated with metabolic rate and thyroid hormone levels (even in euthyroid subjects). Copper and zinc can attenuate the damage that cholesterol feeding causes to rabbits. (Shab-Bidar et al. 2013, Oliver 1975, Alissa et al. 2004, Roos et al. 2007)
Low intake of zinc tends to decrease basal metabolic rate. (Wada&King 1986)
Iron deficiency can also be a problem for some people, but on the other hand, excessive iron could also be a problem, as can be seen from the people with genes causing haemochromatosis (iron overload). (Dillman et al. 1980, Verdon et al. 2003, Edwards et al. 1983)
Obviously, there are plenty of associations between nutrients and thyroid function.
(My note:We can add polyunsaturated fats to this list. PUFA directly and inhibit five independent thyroid functions including synthesis, conversion, transportation, and utilisation. This article offers the details: The Worst Food for Your Thyroid (and Doctors Claim It’s “Essential” to Your Health)
Stress - Those who have read Robert Sapolsky’s popular book Why Zebras Don’t Get Ulcers or any other similar work, are aware of the fact that chronic stress can make one more susceptible to a large amount of diseases. A popular health-blogger, Chris Kresser, has written about some mechanisms of stress-induced hypothyroid symptoms.
Endotoxemia, infections, metabolic syndrome and inflammation - When the lipopolysaccharides (LPS) of gram-negative gut bacteria end up in your bloodstream, the situation/condition is called “endotoxemia.” The most well-known problems caused by endotoxemia are sepsis and liver cirrhosis, but Robert McLeod has written an interesting blog post about how endotoxemia can also disturb the function of thyroid hormones, leading to the decrease of T3 levels and increase of rT3 levels. In rat studies, thyroid hormones protect from the harms of endotoxemia/sepsis. (van der Poll et al. 1999, Yildizdas et al. 2004, Inan et al. 2003)
Endotoxemia does also correlate with atherosclerosis. Inflammatory bowel disease (IBD) is also correlated with CVD, and this association can possibly be explained by the increased endotoxin levels associated with IBD. (Wiedermann et al. 1999, Yarur et al. 2011, Gardiner et al. 1995)
Lately, at least here in Finland, saturated fats have been blamed for TLR-4 activation (leading to inflammation), which seems to be caused by the digestion of fats, in which chylomicrons are featured, leading to postprandial endotoxemia. Clinical data seems to present saturated fats as quite harmless, but if there is some harm involved, endotoxemia could be one possible mechanism. However, quite paradoxically, numerous rodent studies have been conducted in which saturated fats of medium chain length seemed to protect animals from liver damage caused by endotoxemia and lipid peroxidation.**** (Nanji et al. 1997, Nanji et al. 2001, Nanji et al. 1989, Kirpich et al. 2012, Kirpich et al. 2013, You et al. 2005, Li et al. 2013, Ronis et al. 2004, Romestaing et al. 2007)
The composition of a meal might also affect whether the dietary fat causes TLR-4 activation. In one study, orange juice prevented the endotoxin-related inflammation caused by a high-fat meal. (Ghanim et al. 2010)
Fructose is another theoretical cause of endotoxemia. However, high amounts of pure fructose seems to be the real problem, not the moderate amounts of sucrose or fruits. As mentioned above, some forms of fruit (orange juice) might even be able to prevent endotoxemia. Bacterial overgrowth and increased intestinal permeability associated with fructose maldigestion is probably the mechanism for how excess fructose could cause endotoxemia in some people. (Stanhope et al. 2009, Kavanagh et al. 2013, Bergheim et al. 2008, Spruss et al. 2012, Yilmaz 2012, Chesta et al. 1991, Shanab et al. 2011, Miele et al. 2009, Gibson et al. 2007)
Some dietary factors such as dietary antioxidants, choline and glycine, can protect from endotoxemia. Choline can be obtained from liver, egg yolks, milk and meat while bones, cartilage and head cheese are good sources of glycine. Higher consumption of coffee is inversely correlated with liver cirrhosis, but it’s not known whether coffee prevents endotoxemia. (Rivera et al. 1998, Yilmaz et al. 2005, Ilcol et al. 2009, Ilcol et al. 2005, Tvarijonaviciute et al. 2012, Eastin et al. 1997 & Zhong et al. 2003, Yin et al. 1998, Ikejima et al. 1996, Xu et al. 2008, Wang et al. 2013 & Gallus et al. 2002, Klatsky et al. 2006)
There seem to be quite strong correlations between antibodies to certain pathogens (C. pneumoniae, Epstein-Barr virus, herpes simplex virus 2…) and atherosclerosis. (Espinola-Klein et al. 2002, Rupprecht et al. 2001, Taylor-Robinson&Thomas 2000)
Uncontrolled diabetes seems to be associated with significantly decreased T4->T3 conversion in liver, but insulin therapy seems to improve or normalize it. (Islam et al. 2008, Pittman et al. 1979, Saunders et al. 1978)
Many cytokines, protein complexes and other molecules related to inflammation, metabolic syndrome and stress can also have a negative impact on thyroid hormone levels (TNF, IL-1, IL-2, IL-6, IFN, interferon-gamma, cortisol). N-acetyl-cysteine (NAC) might prevent some of IL-6 induced harms, possibly by restoring glutathione levels. (Bartalena et al. 1998 (pdf), Westgren et al. 1977, Stouthard et al. 1994, Corssmit et al. 1995, Nagaya et al. 2000, van der Poll et al. 1990, Kung et al. 1992, Torpy et al. 1998, Bartalena et al. 1994, Abo-Zenah et al. 2008, Boelen et al. 1993, Feelders et al. 1999 & Wajner et al. 2011)
Deficiency of red light and near-infrared radiation - I have written about the fact that red light and near-infrared radiation increase the tissue metabolism and decrease inflammatory cytokines in blood, by activating the mitochondrial enzyme cytochrome c oxidase.
It has been demonstrated in a vast amount of clinical human studies that near-infrared light is a very powerful treatment to various kinds of diseases. Excellent results have been achieved in hypothyroidism, fibromyalgia, osteoarthritis, macular degeneration and many other ailments. In two studies, almost 50% of hypothyroid patients did not require any thyroid medication after the treatment period. (Höfling et al. 2010, Höfling et al. 2013) Moreover, in a Russian study, the diabetic patients' total cholesterol was reduced from 7.98 to 5.31 in one month. (Kovalyova 2002) In cholesterol-fed rabbits, polarized light provides much a stronger protection from atherosclerosis than a statin drug. (Park et al. 2012)
Because higher exposure to near-infrared light seems to be beneficial to health, we can assume that a large percentage of population is getting too little of it. Some of the best sources of near-infrared radiation are sunlight, incandescent lamps, heat lamps and low-level laser therapy (LLLT), which is the most common treatment used in the studies.
11. Other potential benefits of desiccated thyroid therapy
In 1976, Broda Barnes published his book Hypothyroidism: The Unsuspected Illness. In the book he claims that there are numerous diseases which often can be cured or relieved with desiccated thyroid. The list includes health problems such as fatigue, migraine, mental health issues, frequent respiratory infections, menstrual irregularities, hypoglycemia, acne, and the vasculary complications of diabetes. Check the Appendix I for some studies about these ailments.
12. Conclusions
Desiccated thyroid, as a medication, has been studied a few times for prophylaxis of heart disease on clinically euthyroid (normal hormone levels) people. Without exception, the results have been very favourable: In the studies, the cardiovascular mortality in thyroid-treated patients has been less than a fourth of normal. The best effect was seen in people with no background of heart disease.
These studies also raise some questions concerning the diagnosis and treatment of hypothyroidism. Modern blood tests seem to leave a significant amount of people with hypothyroid symptoms undiagnosed, so maybe some other tests such as basal temperature, symptoms, basal metabolic rate and total cholesterol, could be useful in the diagnosis of thyroid hormone insufficiency. We should also consider that desiccated thyroid could be a more useful medication than thyroxine monotherapy, and that sometimes the optimal dosage of thyroid hormones will suppress TSH below the “normal” range.
The medical experts do not usually discuss the studies I’ve been talking about here. One plausible reason could be the fact that these studies do not follow the current RCT gold standard. On the other hand, lack of adequate data doesn’t imply lack of efficacy, and we are faced with the problem that to this date the clinical data on this subject seems to point to the direction that desiccated thyroid could be a very valuable tool in the prevention of the heart disease.
Link to the article with references and appendices is here.




