I recently published an article on my blog about the potential benefits of chronic digestive issues and bacterial imbalance in relation to sulfate metabolism. I postulate that chronic IBS/small intestinal overgrowth/gut dysbiosis may be a protective adaptation in response to sulfate deficiency. Many of the ideas I present here relate to the work of Dr Stephanie Seneff, who we recently interviewed on the Health and Wellness Show. The biophysics of sulfate-water interactions are very interesting, and I believe that they may be one of the reasons why sulfate is "prioritised". Unfortunately, even minor exposure to glyphosate and heavy metals (etc) can essentially screw up the body's ability to transport and utilise sulfate. In response to this, it seems evident (to me) that the body can modulate the gut bacteria toward a more "pathogenic" or "pro-inflammatory" state to mitigate some of the issues related to sulfate metabolism.
Instead of transporting sulfate, the body can package sulfur into hydrogen sulfide gas (as a back-up route), which can then be transported around freely. Unfortunately, hydrogen sulfide gas can cause terrible gut/systemic symptoms when in excess. This article hopefully shines light on the way that the body may choose to have gut dysbiosis, just so that it can derived sulfate from the diet safely. To me, this demonstrates a "body intelligence" and cooperation with the microbiome. To be clear, I do not believe that every (or even most) cases are adaptations to sulfate deficiency, however it would seem likely that this probably does occur quite often in cases which are persistent.
I would love to hear your thoughts on this research, so let me know what you think! And I hope that it might point some people who still suffer from gut issues in the right direction. FWIW, I have been following the protocol (mentioned at the end of the article) for two and a half weeks - the result that I can notice is that a persistent patch of dry skin on my face magically disappeared after a couple of days, and has not returned since :)
SIBO is a notoriously difficult condition to successfully treat long-term, however. Relapse rate is high after treatment, with one small study showing a 44% recurrence after nine months (2). For some individuals, one simple round of herbs or antibiotics may be sufficient to permanently relieve symptoms. Whereas for many others, this condition is a recurrent problem which can persist despite attempting various methods of eradication. There are countless cases (which you can view yourself by perusing online forums and health-related groups) of people in whom this condition seems practically impossible to treat. Even with all of the recommended dietary and lifestyle changes, things do not seem to improve for any sustained period of time. Non-responders may be forced to stick to a low FODMAP/GAPS diet simply to manage symptoms because they are unable to tolerate any other foods.
Time to rethink our approach?
The "nuke'em" approach is simply not effective in some instances. I believe that the fundamental issue with this approach is that it is based on the notion that the human body is unable to regulate or modulate the environment within the gut, and therefore needs fixing. This way of looking at the body is almost identical to that of orthodox medicine, where the only difference is that alternative practitioners might use antimicrobial herbs and supplements instead of pharmaceutical drugs. The underlying dynamic is similar whereby people believe that they can outsmart their own physiology through loading themselves with supplements. This is especially true for SIBO or gut dysbiosis. Now, don't get me wrong, antimicrobial gut-healing protocols certainly do have their place and can clearly be very beneficial. I myself have benefited immensely from these kinds of things in the past. However, I believe that, in some cases at least, SIBO is not an error or mistake that needs to be "fixed" through ordinary means like blasting off the microbiome willy-nilly.
According to naturopathic philosophy, the body has the innate wisdom and intelligence to heal itself when provided with the right tools and conditions. We are not yet able to fully comprehend the significance of this concept, but thankfully research is beginning to demonstrate how this might work.
If only as an interesting mental exercise, try to take a step back and take a look at the manifestation of chronic digestive issues through a naturopathic lens. Might the body actually select for the overgrowth of specific "bad" bacteria in the gut to provide it with something that it does not have access to? In other words, can gut dysbiosis be an intended protective and beneficial adaptation?
Can the body modulate the gut bacteria to suit its own needs?
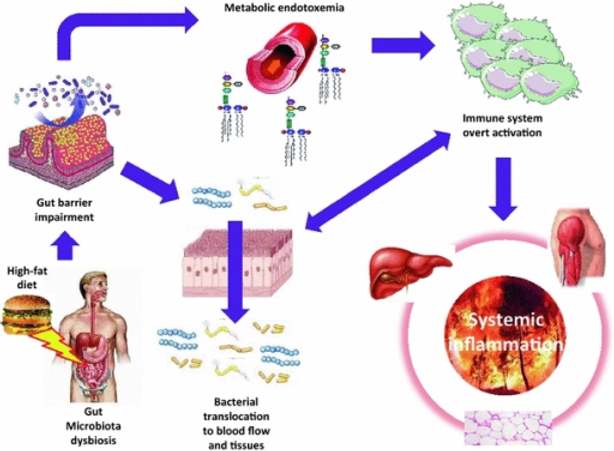
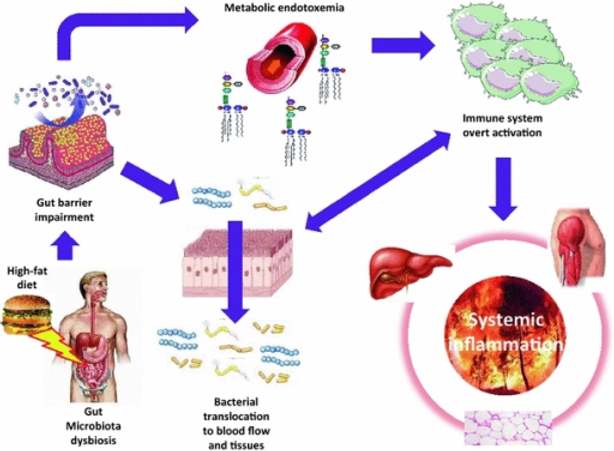
In recent decades an upsurge of scientific research has been published investigating the connection between the microbiome and human health. Researchers have demonstrated potential causal links between imbalances in the gut flora and a wide range of different health conditions, including obesity (3), diabetes (4), autoimmune conditions (5), and even cancers (6). The shift of “healthy” bacterial populations in the gut toward a more “pro-inflammatory” state is accompanied by increases of lipopolysaccharide, a bacterial endotoxin capable of disrupting gut barrier integrity and potentially inducing systemic inflammation. The resulting state of “leaky gut” can then lead to a whole host of other problems.
Furthermore, imbalances in gut bacteria contribute to poor immune function, malabsorption, nutrient deficiencies, and inadequate detoxification (7). Hence, focusing on restoring balance within the gut is a main priority for many practitioners, and rightly so due to its significance for maintaining overall health.
Since the majority of research conducted in this area has highlighted the negative consequences of pro-inflammatory changes in the gut bacteria, dysbiosis is generally considered to be a bad thing. And this is probably correct in many cases. However, there is actually some research which indicates that pro-inflammatory changes in the gut microbiome may serve a beneficial purpose.
One such paper published in 2014 was titled “Adipocyte inflammation is essential for healthy adipose tissue expansion and remodelling.” (8). The study was performed on three mouse models to measure the effects that local inflammation had on adipose tissue expansion and remodelling. To briefly summarise, they demonstrated that pro-inflammatory signalling in the adipocyte (fat cell) was essential for remodelling of the extracellular matrix to allow for more fat to be stored. Impaired adipocyte inflammation led to ectopic lipid accumulation, glucose intolerance, and systemic inflammation. In basic terms, they showed that inflammation in fat tissue prevented metabolic dysfunction! What is more interesting is that the inflammation required for the remodelling process was produced by gut-derived endotoxin.
The authors concluded:
In stark contrast to the idea that “leaky gut” is exclusively detrimental, this study demonstrated pro-inflammatory changes in the gut microbiome were likely a beneficial adaptation to promote survival. So it appears that gut inflammation can be good in a specific context. These findings are also significant because they suggest certain degree of intelligence on the part of the body, and point to the possibility that modulation of gut bacteria may take place to suit the body's needs.
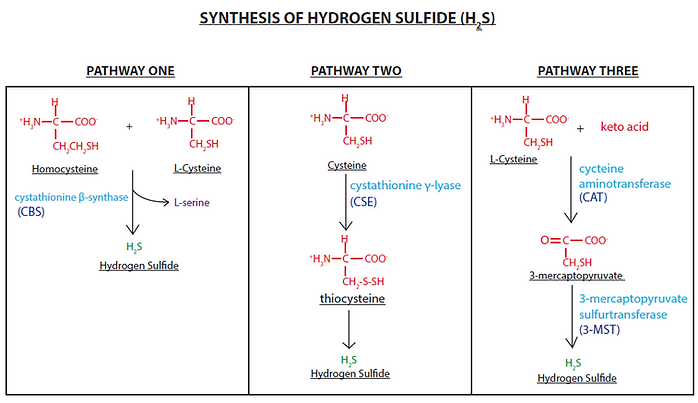
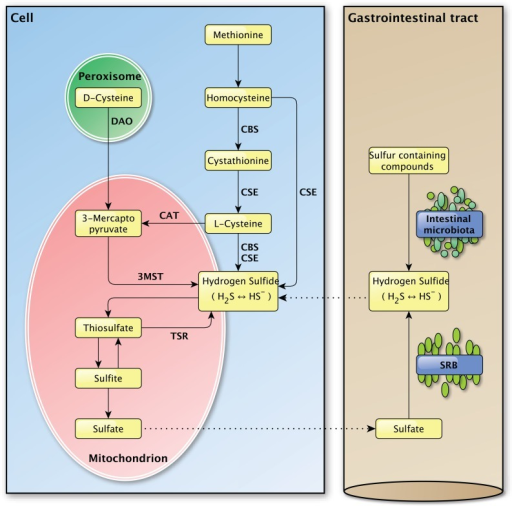
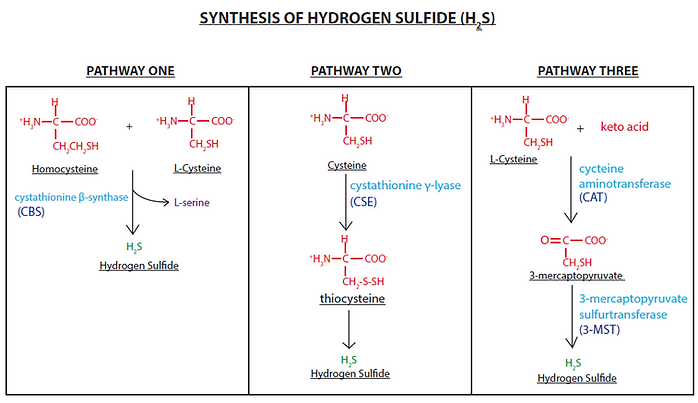
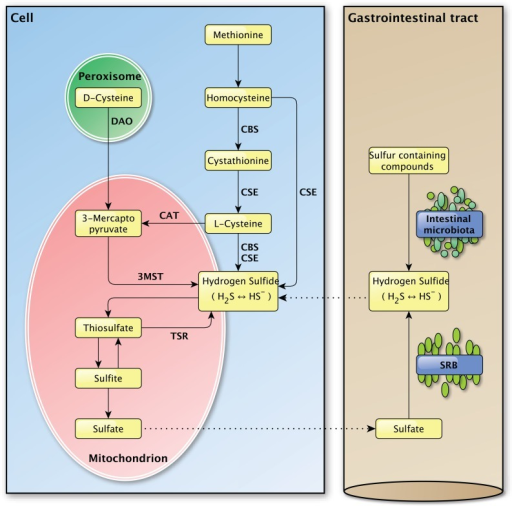
Another study titled “Eukaryotic and prokaryotic contributions to colonic hydrogen sulfide synthesis” (9) set out to measure the contribution of gut bacteria to the total quantity of hydrogen sulfide gas produced in the gut. It is worth noting here that hydrogen sulfide is a gas which is plays many physiological roles (more on this later), and can be produced both by human cells and certain bacteria through a set of reactions (involving CBS and CSE enzymes), using vitamin B6 as a cofactor. Other gut bacteria known as sulfate-reducing bacteria can also synthesise hydrogen sulfide, but instead they do not require these enzymes to do so.
The researchers fed one group of mice a normal diet, and fed the other group a vitamin B6-deficient diet. After two weeks, the fecal content of hydrogen sulfide was significantly reduced in the B6-deficient mice (which was likely due to the inhibition of CBS and CSE enzymes). Though, after six weeks the fecal hydrogen sulfide content returned to the same levels as the control group. In these mice, it is likely that the B6 deficient diet led to an increased growth of the “sulfate reducing bacteria” which are able to produce hydrogen sulfide gas without the need for B6 (9).The author of the study goes on to say “[these findings] may suggest changes in the microflora of these rats or in the production of H2S via alternative pathways by colonic bacteria.” In other words, this was an adaptive response to make up for the deficit of B6 in the diet. The population of gut bacteria shifted to meet the needs of the host.
This looks to me like there is a mutually beneficial relationship between the body and the microbiome, where communication and cooperation seem to be key factors. Is the body choosing to modulate the growth of specific bacteria, or is it the other way round? Perhaps its neither, but it is certainly a fascinating topic!
Is sulfate the missing piece of the puzzle?
Dr Stephanie Seneff and her fellow researchers have written extensively in the past about the possible mutually beneficial dynamics between several so-called "pathogens" and the human body (10). Seneff's work has focused specifically on sulfate's role in physiology and has highlighted the ability of various microorganisms to supply sulfate to the body when it is in low supply. One example is Chlamydia Pnuemoniae. This bacteria has frequently been found to colonise the atheroma in cases of atherosclerosis (11), a finding which led researchers to propose that the infection was potentially a cause of the plaque buildup (12). On the other hand, Seneff and colleagues have suggested the opposite – that the infection may actually be one of the solutions. Those familiar with Seneff's theory of atherosclerosis are probably be aware of the importance of sulfate for the health and maintenance of the cardiovascular system. If you are not familiar with this material then you can read this paper, or alternatively you can refer back to Sulfate III. To summarise, C. Pneumoniae can donate a special type of heparan sulfate to the host cell for use, and Seneff hypothesises that the body may specifically facilitate the passage of this bacterial infection and select for its colonisation to supply the capillary endothelium with sulfate when there are no other options available.
Seneff has also demonstrated the ties between autism and sulfate deficiency in multiple papers. Interestingly enough, statistically significant increases in the presence of C. Pneumoniae in the blood have been detected in autistic children (10). Furthermore, C. Pneumoniae has also been found to be frequently present in the amyloid-beta plaque in patients with Alzheimer's disease. Wendy A. Morely suggested that it may be playing a similar role in sulfate renewal in one review (13): "Chlamydia pneumoniae produce a variant of HS using a set of enzymes that are unique to that species, which suggests that their presence in the brain may have a beneficial role in providing HS to the neural tissues."
The notion that the body would specifically facilitate the passage and colonisation of potential “pathogenic” bacteria to help out may seem like a radical idea. But if we return back to basic naturopathic principles, then it might start to make sense. After all, the body seems to have an innate awareness of what it needs, and the survival of the microbiome depends on the survival of the host.
So if this were the in fact case, then could chronic SIBO/dysbiosis also be an adaptive response to supply extra sulfate?
SIBO/dysbiosis as a way of supplying sulfate against all odds
If you have read the previous three articles in this series, you should be able to appreciate the role that sulfate plays in maintaining the living state. Without sulfate, the blood likely cannot flow. Similarly, the cell is probably unable to perform many other functions. In Sulfate III, I emphasised the likelihood that sulfation is prioritised at the detriment of other processes. Simply put, without adequate sulfate in the vasculature and attached to the cells floating around in the blood, the blood would clot and we would die shortly thereafter.
For a brief overview of the events that should ordinarily take place during the metabolism of sulfur-containing foods, I will refer the reader back to Sulfate I: The Basics. The metabolism of sulfur involves many complex processes and there are multiple steps which can become disrupted. Thankfully, Dr Seneff and colleagues have elucidated several ways in which this pathway can become royally screwed simply by minor exposure to fairly common environmental toxins. The defects in sulfur metabolism might involve cofactor deficiency, enzyme insufficiency or lack of transportation methods (amongst other things).
So when the “ordinary routes” of sulfur transport and metabolism are not working correctly, the body must find other ways to accomplish the task efficiently. Hence, there appears to be a variety of "back-up mechanisms" to do this which involve modulating the gut bacteria toward a more "dysbiotic" and pro-inflammatory state. One such pathway to transport sulfate is through the bacterial synthesis of hydrogen sulfide gas.
Minor introduction to hydrogen sulfide
Aside from hydrogen and methane, SIBO may feature significant quantities of hydrogen sulfide gas production. In fact, the authors of one study even concluded that hydrogen sulfide breath testing could be a more accurate way of diagnosing SIBO than standard breath tests (14). Studies suggest that physiological levels of hydrogen sulfide may play important roles in maintaining the gut-blood-barrier, modulating the inflammatory response, modulating vascular/circulatory homeostasis, and promoting colonic mucous production. The gas can also be oxidised by colonic cells as an energy source to produce ATP. Unfortunately, however, excess levels have been implicated in the pathogenesis of colonic inflammation, IBS, IBD (crohn’s, ulcerative colitis), and bowel cancer (15).
As I briefly mentioned above, hydrogen sulfide can be produced by a variety of bacteria in the gut. The sulfate-reducing bacteria (SRB) are ubiquitous in the mammalian colon and are predominantly comprised of Desulfovibrio, Desulfobacter, Desulfobulbus, and Desulfotomaculu genera. These bacteria non-enzymatically use sulfate and sulfite to fuel their metabolism, with hydrogen sulfide gas yielded as a byproduct. In order to utilise sulfate/sulfite, SRB also require an electron donor such as hydrogen (so we might also assume that hydrogen-dominant SIBO provides abundant substrate for SRB overgrowth). SRB derive sulfur from dietary sources, but can also co-colonize other bacteria which are able break down the mucopolysaccharides in the gut lining as another source of sulfur (16). Not only do SRB promote the breakdown of the gut lining, but the hydrogen sulfide gas is also able to directly induce "leaky gut".
The second source of hydrogen sulfide in the gut comes from the enzymatic conversion of the amino acid cysteine. This can be performed either by the colonic tissues, or by specific anaerobic bacteria such as E.coli, Salmonella enterica, Clostridia, and Enterobacter aerogenes. Additionally, Helicobacter Pylori has been shown to generate hydrogen sulfide (17), while other gut bacteria (E.coli, Klebsiella, Bacillus, Staphylococcus, Coryn, and Rhodococcus ) can also generate the gas by assimilatory sulfite reduction (via sulfite reductase). Researchers have suggested that the majority of H2S production occurs in the upper digestive tract (stomach and small intestine) rather than the colon.
Hydrogen sulfide is a safer alternative to sulfite overload
Hydrogen sulfide can cause some pretty nasty effects when found in higher quantities, so how might this benefit the body? To answer this question, we need to examine some of the things that can go wrong with sulfur metabolism first of all.
Sulfite is an intermediate in sulfur metabolism, but can also be ingested via dietary sources. Sulfite is extremely toxic and can lead to significant oxidative damage, so it is important that the body rapidly converts it to sulfate. The sulfite-to-sulfate conversion relies on an enzyme called sulfite oxidase (SUOX) which uses molybdenum as a cofactor. If this enzyme is not working properly, it can lead to two problems:
Possible factors disrupting the SUOX enzyme include:
In the event of SUOX enzyme inhibition/deficiency, the body faces a potential catastrophe where sulfite is the main offender.
To compound this issue, the enzyme (assimilatory sulfite reductase) responsible for the bacterial synthesis of methionine from sulfite is also busted by glyphosate. Methionine is an essential amino acid, meaning that it must either come from dietary sources or from bacterial synthesis. Glyphosate’s inhibitory action on this enzyme can further contribute toward the excess of sulfite, and may also potentially lead to insufficient methionine. Therefore, in this scenario the body must find another way to dispose of the toxic build-up of sulfite in the gut. Thankfully, many of our bacteria can do this job for us.
According to Seneff et al (18) :
Recall the study I mentioned at the start of the article which showed that the microbiome of vitmain B6-deficient mice adapted by increasing the growth of sulfate-reducing bacteria. I believe that a similar mechanism could occur as an adaptation to poor sulfur metabolism. Interestingly, an overgrowth of Desulfovibrio has been shown to frequently occur in cases of autism (which Seneff believes to be related to sulfate deficiency).
The sulfate-reducing bacteria can take sulfite (very toxic) and convert it to hydrogen sulfide (much less toxic). Hydrogen sulfide can conveniently be rapidly oxidised back into sulfate when it has reached the target tissue via the sulfide-quinone-reductaseenzyme. The main targets for hydrogen sulfide appear to be the liver, the pancreas, and the spinal column.
So, not only does this method reduce the toxic burden of sulfite, but it is also an ingenious method of transporting sulfate around the body when transport methods are limited.
Issues with sulfate transport
One paper titled “Glyphosate’s Suppression of Cytochrome P450 Enzymes and Amino Acid Biosynthesis by the Gut Microbiome: Pathways to Modern Diseases” by Samsel and Seneff highlights the possibility that glyphosate contamination in the vasculature may potentially hamper the route of free sulfate in the blood. Like sulfate, glyphosate is also a strong anionic kosmotrope with the ability to structure surrounding water molecule (see Sulfate III for more details).
According to the authors, the presence of glyphosate in the hepatic portal vein can disrupt the transport of free sulfate from the gut to the liver. The elevated kosmotropic load (due to glyphosate’s kosmotropic properties) means that free sulfate transport would potentially “gel up” the blood excessively, and therefore would be too dangerous.
As a back-up route, chemically suitable compounds such as phenols can diffuse the kosmotropic properties of sulfate, and so can be utilised to transport sulfate through the blood even in the presence of glyphosate in the vasculature . Aromatic amino acids can be metabolised by bacteria in the gut to produce a variety of phenols suitable for this purpose. Unfortunately, many of these bacterial derived phenols become toxic once they have “dropped off” the sulfate to the liver, and so will inevitably cause some damage.
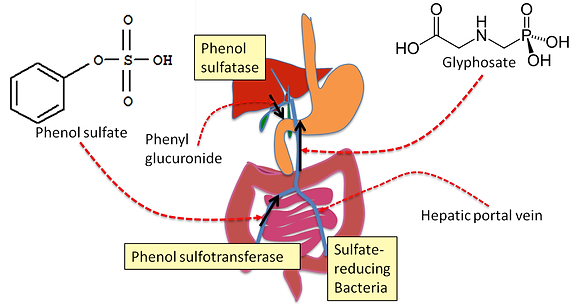
Interestingly, organic acids testing shows that people suffering from gut dysbiosis/SIBO often have elevated phenol markers (such as P-Cresol, HPHPA), as do autistic children and patients with schizophrenia. Elevated phenols usually indicate “pathogenic overgrowth” of certain strains within the Clostridia family of bacteria. They are known to negatively impact dopamine metabolism and produce significant oxidative damage (19). However, despite their toxic effects, these phenols may actually be playing a beneficial role in sulfate transport. Hence, this may be another example of the cooperative relationship between the body and the microbiome in times of stress.
As I said before, hydrogen sulfide can be oxidised directly in the tissue via SQR back to sulfate. In other words, this can be a back-up mechanism for transporting sulfate when there is no other option.
It would therefore make sense that, in response to toxicity-induced enzymatic dysfunction and lack transportation, an adaptive response by the body would foster an overgrowth of sulfate-reducing bacteria and also other "pathogens" such as Clostridia. It seems as though this process of adaptive-dysbiosis is multifaceted and could manifest in several different ways based on each individual. It could feature either an overgrowth of SRB, assimilatory sulfite reducers like E.Coli, phenol producers like Clostridia, or even all three.
As a side note, it is interesting that SIBO is significantly correlated with cardiovascular disease. It has been shown to be more prevalent in coronary artery disease (20), deep vein thrombosis (21) and atherosclerosis (22). Of course, this association can be accounted for by several different mechanisms. However, when placed in the context of Dr Seneff's work on sulfate and its relationship with cardiovascular dysfunction, it is perhaps possible that some of the pro-inflammatory changes in gut flora could be contributing to this back-up supply of sulfate.
I would like to make it clear that glyphosate, heavy metal toxicity, and all of the other influences which contribute to gut dysbiosis can independently induce these effects alone, and that I do not believe that every single case of SIBO is an adaptive response to supply sulfate. For many people, it may have nothing to do with sulfate. SIBO and gut dysbiosis can essentially wreak havoc on the body, and so it is essential that we aim to optimise digestion and overall gut health.
However, it makes inherent sense to me that the body attempts to make the best possible decisions based on the limited options available to it in times of stress. As a last ditch attempt to supply sulfate, I think it is possible that the body will sacrifice other functions which are considered to be non-essential for immediate survival. Something that appears to be pathological may actually be part of the solution.
Benefits of dysbiosis in the context of replenishing sulfate
To summarise, below are some of the potential benefits of bacterial overgrowth when sulfate metabolism is not working properly:
Some practical solutions
As I already mentioned, the metabolism of sulfur is complex. Not only does it involve all of the enzymes directly related to sulfur, it also can be negatively affected if there are disruptions in other pathways like methylation. Thankfully, that aspect of things has been explained thoroughly in many other places and is way beyond the scope of this article. Here, I would just like to briefly outline some of the things that people can do which may help to alleviate some of their health problems. The recommendations below are taken from Dr Greg Nigh and colleagues who have developed a protocol designed for people with poor sulfur metabolism.
If one of the following applies to you, then you may have an issue metabolising sulfur:
Dr Nigh claims to have successfuly treated many cases of SIBO with a protocol which involves an initial period of sulfur exclusion from the diet. He claims that many of the horrible symptoms associated with this issue are due to the negative side-effects of excess hydrogen sulfide. In conjunction with a low sulfur diet, him and his colleagues implement a supplement regime which involves the use of:
At the same time, it is recommended that people take at least 2-3 baths with 4 cups of epsom salts per week. Epsom salts contain both magnesium and sulfate. Trans-dermal sulfate bypasses the gut (where it would usually be converted into hydrogen sulfide), and so is an effective way to deliver sulfate without experiencing symptoms caused by the hydrogen sulfide.After two weeks of sulfur-exclusion, people gradually can introduce sulfur containing foods one by one whilst simultaneously supporting the sulfur pathway with the supplements. This approach has apparently benefited people with both hydrogen and methane dominant SIBO.
Another key point is to avoid glyphosate at all costs! This means to eat organic where ever possible. When organic is not an option, at least stay away from foods heavily sprayed with glyphosate - corn soy, wheat, chickpeas, lentils etc. It may also be advisable to get tested for glyphosate contamination. Similarly, heavy metal toxicity may also be a contributing factor. If you suspect that to be the case, then would be wise to undertake necessary steps in that direction (testing and chelation under the supervision of a knowledgeable a practitioner).
Instead of transporting sulfate, the body can package sulfur into hydrogen sulfide gas (as a back-up route), which can then be transported around freely. Unfortunately, hydrogen sulfide gas can cause terrible gut/systemic symptoms when in excess. This article hopefully shines light on the way that the body may choose to have gut dysbiosis, just so that it can derived sulfate from the diet safely. To me, this demonstrates a "body intelligence" and cooperation with the microbiome. To be clear, I do not believe that every (or even most) cases are adaptations to sulfate deficiency, however it would seem likely that this probably does occur quite often in cases which are persistent.
I would love to hear your thoughts on this research, so let me know what you think! And I hope that it might point some people who still suffer from gut issues in the right direction. FWIW, I have been following the protocol (mentioned at the end of the article) for two and a half weeks - the result that I can notice is that a persistent patch of dry skin on my face magically disappeared after a couple of days, and has not returned since :)
Sulfate IV: Chronic SIBO/Gut Dysbiosis As A Protective Adaptation To Supply Sulfate

Small intestinal bacterial overgrowth (SIBO) is a condition which falls under the umbrella of "gut dysbiosis". As the name implies, it is characterised by an overgrowth of microflora in the small intestine. The typical symptoms include bloating, abdominal pain, excessive foul flatulence, burping, IBS, constipation, diarrhoea, halitosis, acne, etc. The bacteria which colonise this portion of the digestive tract are able to metabolise fermentable fibres to yield significant quantities of gas as a byproduct of metabolism (1). The two predominant gases are hydrogen and methane. The diagnosis of SIBO is based on a test which involves the consumption of a sugar-based solution and then a measurement of the contents of the breath. Elevated levels of either hydrogen or methane gas indicates that there is an overgrowth of bacteria, and is used as evidence to support the adoption of a protocol designed to kill off the bacteria. Protocols typically involve prokinetic agents, digestive enzymes, biofilm disruptors, antimicrobial botanical herbs, antibiotics like rifaximin, and perhaps probiotics as well. Aside from being prescribed a wide array of supplements, people are often told to adopt a low FODMAPs diet or a more restrictive GAPS-type protocol to "starve the bacteria", minimise symptoms and support gut barrier integrity.

Small intestinal bacterial overgrowth (SIBO) is a condition which falls under the umbrella of "gut dysbiosis". As the name implies, it is characterised by an overgrowth of microflora in the small intestine. The typical symptoms include bloating, abdominal pain, excessive foul flatulence, burping, IBS, constipation, diarrhoea, halitosis, acne, etc. The bacteria which colonise this portion of the digestive tract are able to metabolise fermentable fibres to yield significant quantities of gas as a byproduct of metabolism (1). The two predominant gases are hydrogen and methane. The diagnosis of SIBO is based on a test which involves the consumption of a sugar-based solution and then a measurement of the contents of the breath. Elevated levels of either hydrogen or methane gas indicates that there is an overgrowth of bacteria, and is used as evidence to support the adoption of a protocol designed to kill off the bacteria. Protocols typically involve prokinetic agents, digestive enzymes, biofilm disruptors, antimicrobial botanical herbs, antibiotics like rifaximin, and perhaps probiotics as well. Aside from being prescribed a wide array of supplements, people are often told to adopt a low FODMAPs diet or a more restrictive GAPS-type protocol to "starve the bacteria", minimise symptoms and support gut barrier integrity.
SIBO is a notoriously difficult condition to successfully treat long-term, however. Relapse rate is high after treatment, with one small study showing a 44% recurrence after nine months (2). For some individuals, one simple round of herbs or antibiotics may be sufficient to permanently relieve symptoms. Whereas for many others, this condition is a recurrent problem which can persist despite attempting various methods of eradication. There are countless cases (which you can view yourself by perusing online forums and health-related groups) of people in whom this condition seems practically impossible to treat. Even with all of the recommended dietary and lifestyle changes, things do not seem to improve for any sustained period of time. Non-responders may be forced to stick to a low FODMAP/GAPS diet simply to manage symptoms because they are unable to tolerate any other foods.
Time to rethink our approach?
The "nuke'em" approach is simply not effective in some instances. I believe that the fundamental issue with this approach is that it is based on the notion that the human body is unable to regulate or modulate the environment within the gut, and therefore needs fixing. This way of looking at the body is almost identical to that of orthodox medicine, where the only difference is that alternative practitioners might use antimicrobial herbs and supplements instead of pharmaceutical drugs. The underlying dynamic is similar whereby people believe that they can outsmart their own physiology through loading themselves with supplements. This is especially true for SIBO or gut dysbiosis. Now, don't get me wrong, antimicrobial gut-healing protocols certainly do have their place and can clearly be very beneficial. I myself have benefited immensely from these kinds of things in the past. However, I believe that, in some cases at least, SIBO is not an error or mistake that needs to be "fixed" through ordinary means like blasting off the microbiome willy-nilly.
According to naturopathic philosophy, the body has the innate wisdom and intelligence to heal itself when provided with the right tools and conditions. We are not yet able to fully comprehend the significance of this concept, but thankfully research is beginning to demonstrate how this might work.
If only as an interesting mental exercise, try to take a step back and take a look at the manifestation of chronic digestive issues through a naturopathic lens. Might the body actually select for the overgrowth of specific "bad" bacteria in the gut to provide it with something that it does not have access to? In other words, can gut dysbiosis be an intended protective and beneficial adaptation?
Can the body modulate the gut bacteria to suit its own needs?
In recent decades an upsurge of scientific research has been published investigating the connection between the microbiome and human health. Researchers have demonstrated potential causal links between imbalances in the gut flora and a wide range of different health conditions, including obesity (3), diabetes (4), autoimmune conditions (5), and even cancers (6). The shift of “healthy” bacterial populations in the gut toward a more “pro-inflammatory” state is accompanied by increases of lipopolysaccharide, a bacterial endotoxin capable of disrupting gut barrier integrity and potentially inducing systemic inflammation. The resulting state of “leaky gut” can then lead to a whole host of other problems.
Furthermore, imbalances in gut bacteria contribute to poor immune function, malabsorption, nutrient deficiencies, and inadequate detoxification (7). Hence, focusing on restoring balance within the gut is a main priority for many practitioners, and rightly so due to its significance for maintaining overall health.
Since the majority of research conducted in this area has highlighted the negative consequences of pro-inflammatory changes in the gut bacteria, dysbiosis is generally considered to be a bad thing. And this is probably correct in many cases. However, there is actually some research which indicates that pro-inflammatory changes in the gut microbiome may serve a beneficial purpose.
One such paper published in 2014 was titled “Adipocyte inflammation is essential for healthy adipose tissue expansion and remodelling.” (8). The study was performed on three mouse models to measure the effects that local inflammation had on adipose tissue expansion and remodelling. To briefly summarise, they demonstrated that pro-inflammatory signalling in the adipocyte (fat cell) was essential for remodelling of the extracellular matrix to allow for more fat to be stored. Impaired adipocyte inflammation led to ectopic lipid accumulation, glucose intolerance, and systemic inflammation. In basic terms, they showed that inflammation in fat tissue prevented metabolic dysfunction! What is more interesting is that the inflammation required for the remodelling process was produced by gut-derived endotoxin.
The authors concluded:
""Adipose tissue inflammation is therefore an adaptive response that enables safe storage of excess nutrients and contributes to a visceral depot barrier that effectively filters gut-derived endotoxin.
In stark contrast to the idea that “leaky gut” is exclusively detrimental, this study demonstrated pro-inflammatory changes in the gut microbiome were likely a beneficial adaptation to promote survival. So it appears that gut inflammation can be good in a specific context. These findings are also significant because they suggest certain degree of intelligence on the part of the body, and point to the possibility that modulation of gut bacteria may take place to suit the body's needs.
Another study titled “Eukaryotic and prokaryotic contributions to colonic hydrogen sulfide synthesis” (9) set out to measure the contribution of gut bacteria to the total quantity of hydrogen sulfide gas produced in the gut. It is worth noting here that hydrogen sulfide is a gas which is plays many physiological roles (more on this later), and can be produced both by human cells and certain bacteria through a set of reactions (involving CBS and CSE enzymes), using vitamin B6 as a cofactor. Other gut bacteria known as sulfate-reducing bacteria can also synthesise hydrogen sulfide, but instead they do not require these enzymes to do so.
The researchers fed one group of mice a normal diet, and fed the other group a vitamin B6-deficient diet. After two weeks, the fecal content of hydrogen sulfide was significantly reduced in the B6-deficient mice (which was likely due to the inhibition of CBS and CSE enzymes). Though, after six weeks the fecal hydrogen sulfide content returned to the same levels as the control group. In these mice, it is likely that the B6 deficient diet led to an increased growth of the “sulfate reducing bacteria” which are able to produce hydrogen sulfide gas without the need for B6 (9).The author of the study goes on to say “[these findings] may suggest changes in the microflora of these rats or in the production of H2S via alternative pathways by colonic bacteria.” In other words, this was an adaptive response to make up for the deficit of B6 in the diet. The population of gut bacteria shifted to meet the needs of the host.
This looks to me like there is a mutually beneficial relationship between the body and the microbiome, where communication and cooperation seem to be key factors. Is the body choosing to modulate the growth of specific bacteria, or is it the other way round? Perhaps its neither, but it is certainly a fascinating topic!
Is sulfate the missing piece of the puzzle?
Dr Stephanie Seneff and her fellow researchers have written extensively in the past about the possible mutually beneficial dynamics between several so-called "pathogens" and the human body (10). Seneff's work has focused specifically on sulfate's role in physiology and has highlighted the ability of various microorganisms to supply sulfate to the body when it is in low supply. One example is Chlamydia Pnuemoniae. This bacteria has frequently been found to colonise the atheroma in cases of atherosclerosis (11), a finding which led researchers to propose that the infection was potentially a cause of the plaque buildup (12). On the other hand, Seneff and colleagues have suggested the opposite – that the infection may actually be one of the solutions. Those familiar with Seneff's theory of atherosclerosis are probably be aware of the importance of sulfate for the health and maintenance of the cardiovascular system. If you are not familiar with this material then you can read this paper, or alternatively you can refer back to Sulfate III. To summarise, C. Pneumoniae can donate a special type of heparan sulfate to the host cell for use, and Seneff hypothesises that the body may specifically facilitate the passage of this bacterial infection and select for its colonisation to supply the capillary endothelium with sulfate when there are no other options available.
Seneff has also demonstrated the ties between autism and sulfate deficiency in multiple papers. Interestingly enough, statistically significant increases in the presence of C. Pneumoniae in the blood have been detected in autistic children (10). Furthermore, C. Pneumoniae has also been found to be frequently present in the amyloid-beta plaque in patients with Alzheimer's disease. Wendy A. Morely suggested that it may be playing a similar role in sulfate renewal in one review (13): "Chlamydia pneumoniae produce a variant of HS using a set of enzymes that are unique to that species, which suggests that their presence in the brain may have a beneficial role in providing HS to the neural tissues."
The notion that the body would specifically facilitate the passage and colonisation of potential “pathogenic” bacteria to help out may seem like a radical idea. But if we return back to basic naturopathic principles, then it might start to make sense. After all, the body seems to have an innate awareness of what it needs, and the survival of the microbiome depends on the survival of the host.
So if this were the in fact case, then could chronic SIBO/dysbiosis also be an adaptive response to supply extra sulfate?
SIBO/dysbiosis as a way of supplying sulfate against all odds
If you have read the previous three articles in this series, you should be able to appreciate the role that sulfate plays in maintaining the living state. Without sulfate, the blood likely cannot flow. Similarly, the cell is probably unable to perform many other functions. In Sulfate III, I emphasised the likelihood that sulfation is prioritised at the detriment of other processes. Simply put, without adequate sulfate in the vasculature and attached to the cells floating around in the blood, the blood would clot and we would die shortly thereafter.
For a brief overview of the events that should ordinarily take place during the metabolism of sulfur-containing foods, I will refer the reader back to Sulfate I: The Basics. The metabolism of sulfur involves many complex processes and there are multiple steps which can become disrupted. Thankfully, Dr Seneff and colleagues have elucidated several ways in which this pathway can become royally screwed simply by minor exposure to fairly common environmental toxins. The defects in sulfur metabolism might involve cofactor deficiency, enzyme insufficiency or lack of transportation methods (amongst other things).
So when the “ordinary routes” of sulfur transport and metabolism are not working correctly, the body must find other ways to accomplish the task efficiently. Hence, there appears to be a variety of "back-up mechanisms" to do this which involve modulating the gut bacteria toward a more "dysbiotic" and pro-inflammatory state. One such pathway to transport sulfate is through the bacterial synthesis of hydrogen sulfide gas.
Minor introduction to hydrogen sulfide
Aside from hydrogen and methane, SIBO may feature significant quantities of hydrogen sulfide gas production. In fact, the authors of one study even concluded that hydrogen sulfide breath testing could be a more accurate way of diagnosing SIBO than standard breath tests (14). Studies suggest that physiological levels of hydrogen sulfide may play important roles in maintaining the gut-blood-barrier, modulating the inflammatory response, modulating vascular/circulatory homeostasis, and promoting colonic mucous production. The gas can also be oxidised by colonic cells as an energy source to produce ATP. Unfortunately, however, excess levels have been implicated in the pathogenesis of colonic inflammation, IBS, IBD (crohn’s, ulcerative colitis), and bowel cancer (15).
As I briefly mentioned above, hydrogen sulfide can be produced by a variety of bacteria in the gut. The sulfate-reducing bacteria (SRB) are ubiquitous in the mammalian colon and are predominantly comprised of Desulfovibrio, Desulfobacter, Desulfobulbus, and Desulfotomaculu genera. These bacteria non-enzymatically use sulfate and sulfite to fuel their metabolism, with hydrogen sulfide gas yielded as a byproduct. In order to utilise sulfate/sulfite, SRB also require an electron donor such as hydrogen (so we might also assume that hydrogen-dominant SIBO provides abundant substrate for SRB overgrowth). SRB derive sulfur from dietary sources, but can also co-colonize other bacteria which are able break down the mucopolysaccharides in the gut lining as another source of sulfur (16). Not only do SRB promote the breakdown of the gut lining, but the hydrogen sulfide gas is also able to directly induce "leaky gut".
The second source of hydrogen sulfide in the gut comes from the enzymatic conversion of the amino acid cysteine. This can be performed either by the colonic tissues, or by specific anaerobic bacteria such as E.coli, Salmonella enterica, Clostridia, and Enterobacter aerogenes. Additionally, Helicobacter Pylori has been shown to generate hydrogen sulfide (17), while other gut bacteria (E.coli, Klebsiella, Bacillus, Staphylococcus, Coryn, and Rhodococcus ) can also generate the gas by assimilatory sulfite reduction (via sulfite reductase). Researchers have suggested that the majority of H2S production occurs in the upper digestive tract (stomach and small intestine) rather than the colon.
Hydrogen sulfide is a safer alternative to sulfite overload
Hydrogen sulfide can cause some pretty nasty effects when found in higher quantities, so how might this benefit the body? To answer this question, we need to examine some of the things that can go wrong with sulfur metabolism first of all.
Sulfite is an intermediate in sulfur metabolism, but can also be ingested via dietary sources. Sulfite is extremely toxic and can lead to significant oxidative damage, so it is important that the body rapidly converts it to sulfate. The sulfite-to-sulfate conversion relies on an enzyme called sulfite oxidase (SUOX) which uses molybdenum as a cofactor. If this enzyme is not working properly, it can lead to two problems:
- The toxic build-up of sulfite
- Sulfate deficiency
Possible factors disrupting the SUOX enzyme include:
- Molybdenum deficiency: The common herbicide Glyphosate (round-up ready) is a potent chelator of molybdenum.
- Glyphosate substitution for glycine in protein synthesis: The SUOX enzyme contains critical glycine residues which could theoretically be replaced by glyphosate during protein synthesis - a process which may render the SUOX enzyme dysfunctional.
- Mercury and Lead toxicity: These interfere with enzyme function.
- SUOX genetic polymorphism: A single nucleotide polymorphism in the SUOX gene may interfere with the speed and efficiency by which this enzyme can perform its function.
In the event of SUOX enzyme inhibition/deficiency, the body faces a potential catastrophe where sulfite is the main offender.
To compound this issue, the enzyme (assimilatory sulfite reductase) responsible for the bacterial synthesis of methionine from sulfite is also busted by glyphosate. Methionine is an essential amino acid, meaning that it must either come from dietary sources or from bacterial synthesis. Glyphosate’s inhibitory action on this enzyme can further contribute toward the excess of sulfite, and may also potentially lead to insufficient methionine. Therefore, in this scenario the body must find another way to dispose of the toxic build-up of sulfite in the gut. Thankfully, many of our bacteria can do this job for us.
According to Seneff et al (18) :
"A deficiency in sulfite oxidase would encourage the growth of microbes able to reduce highly toxic sulfite to less toxic H2S, which would then disrupt the tight barrier that keeps the microbes and the toxins they produce from penetrating into the general circulation.
[..]
One can hypothesize that, as a consequence of E. coli’s impaired ability to incorporate the sulfur atom of sulfite into organic sulfur compounds, the dissimilatory sulfite reductase of Desulfovibrio produces H2S from sulfite instead."
Recall the study I mentioned at the start of the article which showed that the microbiome of vitmain B6-deficient mice adapted by increasing the growth of sulfate-reducing bacteria. I believe that a similar mechanism could occur as an adaptation to poor sulfur metabolism. Interestingly, an overgrowth of Desulfovibrio has been shown to frequently occur in cases of autism (which Seneff believes to be related to sulfate deficiency).
The sulfate-reducing bacteria can take sulfite (very toxic) and convert it to hydrogen sulfide (much less toxic). Hydrogen sulfide can conveniently be rapidly oxidised back into sulfate when it has reached the target tissue via the sulfide-quinone-reductaseenzyme. The main targets for hydrogen sulfide appear to be the liver, the pancreas, and the spinal column.
So, not only does this method reduce the toxic burden of sulfite, but it is also an ingenious method of transporting sulfate around the body when transport methods are limited.
Issues with sulfate transport
One paper titled “Glyphosate’s Suppression of Cytochrome P450 Enzymes and Amino Acid Biosynthesis by the Gut Microbiome: Pathways to Modern Diseases” by Samsel and Seneff highlights the possibility that glyphosate contamination in the vasculature may potentially hamper the route of free sulfate in the blood. Like sulfate, glyphosate is also a strong anionic kosmotrope with the ability to structure surrounding water molecule (see Sulfate III for more details).
According to the authors, the presence of glyphosate in the hepatic portal vein can disrupt the transport of free sulfate from the gut to the liver. The elevated kosmotropic load (due to glyphosate’s kosmotropic properties) means that free sulfate transport would potentially “gel up” the blood excessively, and therefore would be too dangerous.
As a back-up route, chemically suitable compounds such as phenols can diffuse the kosmotropic properties of sulfate, and so can be utilised to transport sulfate through the blood even in the presence of glyphosate in the vasculature . Aromatic amino acids can be metabolised by bacteria in the gut to produce a variety of phenols suitable for this purpose. Unfortunately, many of these bacterial derived phenols become toxic once they have “dropped off” the sulfate to the liver, and so will inevitably cause some damage.
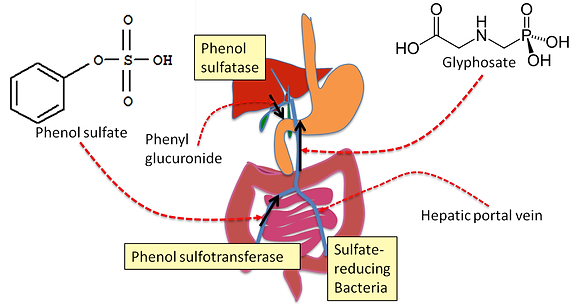
Interestingly, organic acids testing shows that people suffering from gut dysbiosis/SIBO often have elevated phenol markers (such as P-Cresol, HPHPA), as do autistic children and patients with schizophrenia. Elevated phenols usually indicate “pathogenic overgrowth” of certain strains within the Clostridia family of bacteria. They are known to negatively impact dopamine metabolism and produce significant oxidative damage (19). However, despite their toxic effects, these phenols may actually be playing a beneficial role in sulfate transport. Hence, this may be another example of the cooperative relationship between the body and the microbiome in times of stress.
As I said before, hydrogen sulfide can be oxidised directly in the tissue via SQR back to sulfate. In other words, this can be a back-up mechanism for transporting sulfate when there is no other option.
It would therefore make sense that, in response to toxicity-induced enzymatic dysfunction and lack transportation, an adaptive response by the body would foster an overgrowth of sulfate-reducing bacteria and also other "pathogens" such as Clostridia. It seems as though this process of adaptive-dysbiosis is multifaceted and could manifest in several different ways based on each individual. It could feature either an overgrowth of SRB, assimilatory sulfite reducers like E.Coli, phenol producers like Clostridia, or even all three.
As a side note, it is interesting that SIBO is significantly correlated with cardiovascular disease. It has been shown to be more prevalent in coronary artery disease (20), deep vein thrombosis (21) and atherosclerosis (22). Of course, this association can be accounted for by several different mechanisms. However, when placed in the context of Dr Seneff's work on sulfate and its relationship with cardiovascular dysfunction, it is perhaps possible that some of the pro-inflammatory changes in gut flora could be contributing to this back-up supply of sulfate.
I would like to make it clear that glyphosate, heavy metal toxicity, and all of the other influences which contribute to gut dysbiosis can independently induce these effects alone, and that I do not believe that every single case of SIBO is an adaptive response to supply sulfate. For many people, it may have nothing to do with sulfate. SIBO and gut dysbiosis can essentially wreak havoc on the body, and so it is essential that we aim to optimise digestion and overall gut health.
However, it makes inherent sense to me that the body attempts to make the best possible decisions based on the limited options available to it in times of stress. As a last ditch attempt to supply sulfate, I think it is possible that the body will sacrifice other functions which are considered to be non-essential for immediate survival. Something that appears to be pathological may actually be part of the solution.
Benefits of dysbiosis in the context of replenishing sulfate
To summarise, below are some of the potential benefits of bacterial overgrowth when sulfate metabolism is not working properly:
- Neutralising sulfite: Sulfate-reducing bacteria and assimilatory sulfite reducers dispose of excess sulfite to mitigate oxidative damage to cellular components.
- Hydrogen sulfide transport: Sulfate-reducing bacteria can package sulfur into hydrogen sulfide gas which can be absorbed into the bloodstream or can diffuse through tissues to be oxidised on-site back into sulfate.
- Phenol transport: Clostridia and other pathogens produce phenolic compounds (such as HPHPA, P-Cresol etc) which can safely shuttle sulfate through the blood to the liver.
Some practical solutions
As I already mentioned, the metabolism of sulfur is complex. Not only does it involve all of the enzymes directly related to sulfur, it also can be negatively affected if there are disruptions in other pathways like methylation. Thankfully, that aspect of things has been explained thoroughly in many other places and is way beyond the scope of this article. Here, I would just like to briefly outline some of the things that people can do which may help to alleviate some of their health problems. The recommendations below are taken from Dr Greg Nigh and colleagues who have developed a protocol designed for people with poor sulfur metabolism.
If one of the following applies to you, then you may have an issue metabolising sulfur:
- Have tried antimicrobial protocols but still suffer from chronic gut issues - SIBO type symptoms
- Red, hot presentation or symptoms related to heat - flushes, eczema, hives, cystic acne
- Experience any other skin problems
- Experience brainfog, poor concentration and memory
- Poor alcohol tolerance
- Have a reaction to sulfur containing foods like egg, garlic, onion, leek, cruciferous vegetables
Dr Nigh claims to have successfuly treated many cases of SIBO with a protocol which involves an initial period of sulfur exclusion from the diet. He claims that many of the horrible symptoms associated with this issue are due to the negative side-effects of excess hydrogen sulfide. In conjunction with a low sulfur diet, him and his colleagues implement a supplement regime which involves the use of:
- Molybdenum (to support the SUOX enzyme)
- Butyrate (to support gut barrier integrity)
- Zinc acetate (to reduce hydrogen sulfide)
- Sublingual hydroxocobalamin (to bind with hydrogen sulfide)
- Bismuth (to reduce hydrogen sulfide production in the gut)
- Probiotics
At the same time, it is recommended that people take at least 2-3 baths with 4 cups of epsom salts per week. Epsom salts contain both magnesium and sulfate. Trans-dermal sulfate bypasses the gut (where it would usually be converted into hydrogen sulfide), and so is an effective way to deliver sulfate without experiencing symptoms caused by the hydrogen sulfide.After two weeks of sulfur-exclusion, people gradually can introduce sulfur containing foods one by one whilst simultaneously supporting the sulfur pathway with the supplements. This approach has apparently benefited people with both hydrogen and methane dominant SIBO.
Another key point is to avoid glyphosate at all costs! This means to eat organic where ever possible. When organic is not an option, at least stay away from foods heavily sprayed with glyphosate - corn soy, wheat, chickpeas, lentils etc. It may also be advisable to get tested for glyphosate contamination. Similarly, heavy metal toxicity may also be a contributing factor. If you suspect that to be the case, then would be wise to undertake necessary steps in that direction (testing and chelation under the supervision of a knowledgeable a practitioner).
For more information on Dr Nigh's protocol, you can listen to this podcast or watch the video webinar below:

 .
. 

 The only symptom I don't have is the last one on this list. Well, kind of, I can only tolerate small amounts of garlic.
The only symptom I don't have is the last one on this list. Well, kind of, I can only tolerate small amounts of garlic.






 We generally roasted the chicken drumsticks in the oven. With the heart we diced it, added some root veg, water, salt and herbs and put it in the slow cooker over night. I've never really had heart by itself and I must say I was pleasantly surprised! With the fish you could oven bake, fry or grill and have some green veggies on the side.
We generally roasted the chicken drumsticks in the oven. With the heart we diced it, added some root veg, water, salt and herbs and put it in the slow cooker over night. I've never really had heart by itself and I must say I was pleasantly surprised! With the fish you could oven bake, fry or grill and have some green veggies on the side.