Here is a very interesting post that reviews the intricacies of the immune system. Some might find it unreadable, but this author does a pretty nice synthesis while he connects some dots and clues on this difficult subject. First, some basic background on T-regs:
What are T-regs?
Here is the article. The references marked as (R) are hyperlinked in the original article:
What are T-regs?
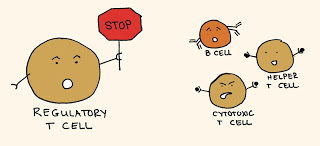
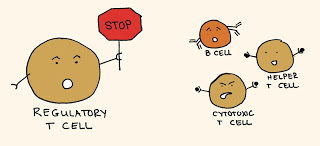
Regulatory T cells
Regulatory T cells (TReg cells) are a special subset of T cells [a type of lymphocyte] that prevent other immune cells from attacking the body’s own tissues and other harmless environmental materials, such as food and commensal organisms. Defects in regulatory T cells cause severe inflammatory disease.
The regulatory T cells (Tregs pronunciation: /ˈtiːrɛɡ/), formerly known as suppressor T cells, are a subpopulation of T cells which modulate the immune system, maintain tolerance to self-antigens, and prevent autoimmune disease.
Here is the article. The references marked as (R) are hyperlinked in the original article:
Tregs: The Missing Link To Cure Autoimmune and Inflammatory Disorders
_https://selfhacked.com/2014/11/11/treg/
If you are having a hard time reading the material, then just read the bolded parts.
Tregs comprise ∼5%–10% of T helper cells and can be identified by the DNA reading protein ‘Foxp3’ or a lot of CD25 proteins on its membrane/surface.
There are two types of Tregs: ‘natural’ (nTregs) or ‘induced’ (iTregs). Both types are anti-inflammatory. Natural means that they are part of the cells naturally found in our thymus gland. Induced means that they are created outside the thymus. (There are 2 kinds of induced Tregs: Tr1 and Th3) (R, R2).
Tregs produce TGF-B and interleukin IL-10, both of which mostly inhibit the immune system (R).
Tregs suppress the harmful/activated (effector) Th1, Th2, Th17 cells and their cytokines, eosinophils, mast cells, basophils, IgE’s (switches to IgG4) and the migration of inflammatory cells to tissues (R).
In addition, they suppress CD8+ T cells, dendritic cells (DCs), monocytes/macrophages, B cells, natural killer cells and natural killer T cells (R).
Tregs need to be ‘activated’ in order to have their suppressor functions (R).
Tregs inhibit immune activation by a direct cell to cell contact. This means that it doesn’t only work through cytokine intermediaries such as TGF-B and IL-10. These cells are directly anti-inflammatory (R). For some reason, this information excites me.
You can test your Treg Cell numbers by taking a blood test. This test doesn’t check for certain important aspects of Treg cells, to my knowledge (Foxp3 nor ‘high’ CD25). However, since these cells are mostly are good against autoimmunity, checking the absolute number of cells should have some value (R).
Checking TGF-B1 and IL-10 (checked in the Th1/Th2/Th17 dominance test) should give a clearer picture as to what your level of Tregs are like. This is because TGF-B1 increases Tregs and IL-10 is given off by Tregs. I’d recommend all three tests to get a decent picture.
Top 8 Picks to Increase Tregs
Probiotics (R) – must be this one. Great referenced article. {Referenced article mentions specifically: Lactobacillus casei (L. casei, Lactobacillus rhamnosus GG, L. casei Shirota, L. salivarius, L. reuteri, L. plantarum, L. paracasei}
Hi-maize /Resistant starch/Butyrate (R, R2, R3, R4)
DHA, vitamin A and vitamin D3 (R, R2)
EGCG/Tea (Jasmine) (R, R2), – DNMT inhibitor (R)
Curcumin (R, R2, R3) – Good for inducing oral tolerance by inducing gut Tregs in multiple ways. It does inhibit the suppressive activity of Tregs, though (R).
Black Cumin Seed Oil (R)
NAC (R) (Clinical Trial)
Cinnamon/Sodium Benzoate (R)

The Good
Treg cells help to restrain the immune system and prevent an excessive T Cell response (R).
Even is healthy people, immune cells can attack our own tissue. Tregs stop our immune cells from attacking our own tissue (R).
In particular, TGFb and IL-10 seem to be crucial for sustained tolerance induction by Treg. (R) On the other hand, TNF, IL-1 and IL-6 block the ability of Tregs to induce tolerance (R).
Tregs can also reverse food intolerances and allergies.
Probably the single most important reason we develop IgE-related allergies is because we aren’t creating Treg cells in the gut, but instead Th2 or Th17 cells (R).
This happens in 3 ways: by changing the type of dendritic cells that reside in our gut, by blocking Th2/mast cells/other immune cells, and by actually changing the tissue structure of our gut (R).
Our gut has dendritic cells that capture proteins from food and bring them to the lymph nodes. To produce Tregs, we need sufficient vitamin A, TGF-B, and the enzyme IDO (R).
If we produce Tregs, then they will tell the dendritic cells that the protein they carry is cool and there’s no need to ring the alarm bells (R).
For oral tolerance, immune cells (DCs) are told not to react to a protein in the gut tissue, and these cells circulate to other tissues, which trains the immune system (R).
Technical: Tregs produce inhibitory cytokines (eg, IL-10, TGFb, and IL-35), absorb inflammatory cytokines, kill target cells directly (secretion of granzymes, perforin), block important cellular functions (through CD25, 39, 73 and adenosine), increase cAMP (and therefore energy), decrease costimulatory molecules (CD80/CD86) and turn the dendritic cells off by activating surface proteins that inhibit immune function (CTLA-4, PD-1, or histamine receptor 2.)” (R, R2).
I’ve tried all different ways to induce tolerance, but I haven’t found this to be effective for lectin sensitivity at all. This works for probably most other food allergies.
Treg cells, surprisingly, can be important for clearing some infections. They are crucial for the establishment of a functional Th17 response after the infection in the gut (with the help of IL-2) (R).
Tregs can improve wound healing (R) and are neuroprotective in stroke models (R).
The Bottom Line: If you’ve got autoimmune or inflammatory problems, there’s a good chance that you’re deficient in Tregs or that they’re dysfunctional. Tregs can then be considered ‘good’.
The Bad
Unrestrained Treg-cell activity can lead to impaired immunity (R), which means high Tregs will make you will be less capable of fighting most infections.
For example, a high level of Tregs can theoretically make people with CFS and other disorders believed to be caused by viral infections worse. Indeed, not surprisingly, people with CFS have higher levels of Tregs. (R)
In my EBV/Mono post, I speak about how various autoimmune disorders can be caused by a viral infection that’s out of control.
Two significant factors that cause this is a low Th1 immune system/low INFy and low cytotoxic T cells (CD8+).
If you have high Tregs, it will decrease both of these immune system aspects, plus others that are involved with keeping viral infections at bay.
So any disorder caused or aggravated by a viral infection should become worse by having high Tregs.
However, if you have high Tregs, it will create tolerance to specific tissues and will, therefore, be overall beneficial when it comes to classical autoimmune disease. And we see this below in the list of diseases with low Tregs.
This may not be the case for something like CFS, though, which is more systemic rather than a specific tissue being attacked as is the case by a classical autoimmune disorder.
Tregs can have a dark side when it comes to cancer because they limit our ability to fight tumors, to a degree. They curtail the generation of Th1 responses. Part of these responses is the production of CD8+/Cytotoxic T cells and IFNy. Both of these fight tumors (R).
Tregs are also the main source of IL-10 in tumors, which I discussed inhibits our ability to kill tumors to some degree (R).
Tregs also inhibit the body’s ability to suppress the formation of cancerous cells (R), which means high Tregs will lead to cancer.
Patients with tumors have a local excess of Tregs (R).
Tregs can also increase inflammation in certain situations because they can become dysfunctional and start producing IL-17 (R).
Bottom Line: If you’ve got cancer, you might want to shift your immune system to decrease Tregs – at least in cancer tissue. However, systemic levels do likely influence levels in cancer tissues.
The Ideal Treg Scenario
The ideal scenario is to have a healthy Treg level throughout your body, but low Treg levels in cancer or precancerous tissue.
Also, ideally, Tregs would be decreased when we have an infection and increase when we get over it.
Why Can’t We Just Inject Tregs Into People?
Unfortunately, recent T cell biology investigations revealed that T cell nature is much more plastic than initially thought (R).
Treg cell therapy may be very risky, as the Treg cells transferred to the patient may reverse and become another proinflammatory Th17 cell (R). IL-10 is a cytokine that blocks this conversion from happening (R).
You see, in these cells, there are two proteins that read the DNA, which command the cell’s activities and produce products: Foxp3 and RORyt. When Foxp3 decreases relative to RORyt, the cell will start producing more IL-17. There’s no dividing line at which Tregs become dark villains; it’s on a continuum (R).
So it’s the level of Foxp3 in the Treg that matters most. In psoriasis, skin cells have lots of Tregs but reduced Foxp3 (R).
The good news is that HDAC inhibitors such as Hi-Maize/Resistant starch/Butyrate block the conversion of healthy Tregs to IL-17 producing Tregs (R).
Tregs are produced under the influence of solely TGF-β. Th17 cells are produced under the influence of TGF-β AND IL-6 or IL-21 (human studies point to IL-21, while mouse studies point to IL-6) (R).
Various cytokines such as IL-1b, IL-2 (Th1 cytokine), IL-23 and IL-15 turn Angelic Tregs to Villain Tregs.
What needs to be done then to heal yourself/prevent disease is to change the environment of these cells. This means to decrease systemic inflammation, ideally by getting to the root cause.
Diseases With Low/Dysfunctional Tregs
Heart Disease/Atherosclerosis (R)
IBS (R)
Diabetes (R)
Sleep apnea (R)
Allergies (R, R2)
IBD (R): Colitis (R), Crohn’s (R).
Rheumatoid arthritis (R) – The function of Treg is known to be suppressed by TNF-α in RA (R)
Multiple sclerosis (R), Type I diabetes (R), SLE (R)
Hashimoto’s (R), Graves (R) – Dysfunctional Tregs, not lower numbers… In Thyroiditis patients, two studies showed no deficit in Treg number, while another study found that only untreated Graves’ patients had a significant decrease in Tregs (R).
Eczema (R), Psoriasis (R).
Gastritis, oophoritis, Prostatitis, Renal disease (R).
Increasing Tregs
Increasing Tregs is a way to benefit both Th1 and Th2 dominance (R). Tregs decrease Th1 cells and help create oral tolerance for Th1/Th2 type allergies.
Inhibiting mTOR results in increased Treg levels (R).
However, studies have found that having variations in mTOR is important for Treg development. So you don’t want to constantly inhibit it; instead, cycle with high and low mTOR activation (R).
The depletion of arginine, glutamine, and tryptophan increases Treg generation (via inhibiting mTOR) (R).
Increasing AMPK also increases Tregs (mTOR article has AMPK activators) (R).
Tregs prefer to burn fat for fuel and when you take this away from them, they are less likely to develop (R).
Oddly, gluten may increase Tregs. Tregs were significantly lower in patients who had abstained from gluten compared with individuals on a standard diet (R). However, I wouldn’t pay much attention to this, because Tregs probably went down as a result of less inflammation (so there needed to be less Tregs)…
Sun/UV (R)
Exercise (R)
Fall in love, have sex, nurse and have positive social encounters. All of these lead to increased oxytocin (R). Oxytocin increases Tregs and wound healing (R)
Circadian Rhythm – if you constantly break the rhythm, you will produce more Th17 instead of Tregs.
alpha-MSH (R)
Polyphenols in general (R)
Oxytocin (R)
L Reuteri – Increases oxytocin also (R)
IGF-1 (R)
Vit A adequacy/Cod liver (R)
Vitamin D3 adequacy/Cod liver (R)
THC/Pot (CB2) (R)
CBD (R)
DHA (R, R2)
Grape Seed Extract (R)
Licorice (R)
Baicalin (R) (Increased Treg numbers, TGF-B, IL-10, and FOXP3) (R)
Honokiol (R) (TGF-B, IL-10, FOXP3)
Naringenin (R)
Astragalus (R, R2) – Increased Foxp3 and decreased that of RORγt. But it decreases TGF and Tregs when exposed to some viruses (R)
Lipoic Acid (R)
Cocoa (R) – prevented a decrease in Tregs…
Whey (R)
Cat’s claw (R)
Papain/Papaya (R)
Probiotics (R)–Lactobacilli (R), Probiotics (L casei, L Reuteri, Lactobacillus rhamnosus Goldin-Gorbach and L. casei Shirota, L. salivarius, IRT5L. plantarum, L. salivarius (R), and L. lactis (R)), B Fragilis (R).
GABA(A) (R)
Nicotine (R) (increases Foxp3, CTLA-4)
Nitric Oxide (R) – arginine, exercise
Exogenous ATP (R)
FOXO3a(+), IDO (R), DPP4 (-) (R), DNMT (-) (R), NFAT hyperactivation (R)….Some ingested immunoreactive proteins type I IFN, SIRS peptide 1–21, α-MSH, ACTH, SST…
Decreasing Tregs
The mTOR–Akt pathway suppresses Treg cell production and activity (R). So you want to inhibit mTOR.
High-fat diet (R) (in mouse livers)
Leptin (R)
Marathons/Excess exercise (R)
Artemisinin (R) – in cancer cells
NAD+? (R)
Melatonin (R) – in tumor tissues
Contradictory/Doesn’t Alter Tregs
Resveratrol (R) – By activating SIRT1, it may block Tregs (R). Prevents high-fat diet decrease in Tregs (R).
Bromelain (R) (Decreases CD25 though)
Berberine (R)
Unknown
Stevia, Blueberry
Oxidative Stress Helps Tolerance…What To Do?
Oxidative stress/ROS actually helps Tregs suppress immune activation. Particularly, NADPH oxidase is important (produces superoxide). In fact, Tregs are able to suppress the secretion of cysteine into the microenvironment by dendritic cells to indirectly suppress T effector proliferation via cysteine depletion (R).
First, there’s no need to worry about molecular hydrogen because that doesn’t affect the free radical superoxide, which is what the study is concerned with.
However, this puts a damper on NAC and Spirulina, both of which inhibit the oxidant in question.
However, I’ve done well on NAC and most clients report positive results.
In addition, many benefits have been reported in a clinical trial: NAC increased mitochondrial membrane potential in all T cells, profoundly reduced mTOR activity, enhanced apoptosis, reversed expansion of CD4−CD8− T cells, stimulated FoxP3 expression in CD4+CD25+ T cells, and reduced anti-DNA production (R). Increased mitochondrial membrane potential leads to the destruction of activated T cells (R).
I think what might be happening here is NAC may briefly decrease the induction of tolerance for a couple of hours. Since it’s brief, it’s not an issue. Otherwise, NAC may behave differently when people ingest it. Whatever the case, I think the benefits outweigh this potential negative.


