Palinurus
The Living Force
Source: More euthanasia cases in 2022, 29 couples helped to die - DutchNews.nl
Similar (but shorter): One in 20 deaths in Netherlands last year was euthanasia
Coverage in Dutch:
Nieuwe piek in cijfers euthanasie: vorig jaar 8720 meldingen
msn.com/nl-nl/nieuws/other/een-op-de-twintig-overlijdens-vorig-jaar-met-euthanasie
Steeds meer mensen kiezen voor euthanasie én krijgen toestemming
More euthanasia cases in 2022, 29 couples helped to die
April 5, 2023
The number of people dying in the Netherlands with the help of euthanasia rose nearly 14% last year to 8,720, according to new figures from the regional monitoring committees, or RTE.
The percentage is higher than in recent years and took the proportion of euthanasia deaths up from 4.5% to 5.1% of all deaths last year. The number of deaths by euthanasia had been increasing by around 10% a year.
No scientific research has been carried out to establish a reason for the increase, the RTE said.
Most euthanasia requests are carried out on people who have cancer, but last year 288 dementia sufferers were helped to die, a rise of 34% on 2021.
‘Euthanasia for people with dementia is a complex and sensitive subject because at a certain point you are no longer mentally competent,’ said Fransien van ter Beek, of the voluntary euthanasia society NVVE. ‘So it is important to make your wishes and boundaries clear in time, and to involve a doctor.’
Couples
A further 379 elderly people died because they were suffering from a multitude of illnesses with no hope of recovery. This is a rise of 23% on 2021. Of them, 58 were part of a couple who chose to die together. In cases like these, both partners have to see a different consultant and both have to fully meet the criteria to be helped to die, the RTE said.
‘Despite the increase, there is a lot of uncertainty among doctors and the wider population about euthanasia and the accumulation of complaints associated with getting old,’ said Van ter Beek. ‘We would like to see more education for doctors on this topic.’
In 115 cases, people with severe psychiatric illness were helped to die, the same number as in 2021.
Criteria
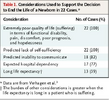
In 13 cases, or 0.15% of the total, the RTE said doctors had not fully met the detailed legal demands when helping someone to die. Since euthanasia was legalized 20 years ago, just 133 of the 91,565 reports had not met the legal criteria.
‘We can draw the cautious conclusion that the legislation and the RTE have achieved what was intended: the caring and transparent practice of euthanasia in the Netherlands,’ said RTE chairman Jeroen Recourt.
To qualify for euthanasia in the Netherlands, the patient must be experiencing unbearable suffering with no prospect of improvement. Two doctors must also be involved, and meet detailed criteria covering duty of care.
Similar (but shorter): One in 20 deaths in Netherlands last year was euthanasia
Coverage in Dutch:
Nieuwe piek in cijfers euthanasie: vorig jaar 8720 meldingen
msn.com/nl-nl/nieuws/other/een-op-de-twintig-overlijdens-vorig-jaar-met-euthanasie
Steeds meer mensen kiezen voor euthanasie én krijgen toestemming