You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Coronavirus Pandemic: Apocalypse Now! Or exaggerated scare story?
- Thread starter wanderingthomas
- Start date
Don't know if this has been posted or not - I have to FLY over this thread half the time because it grows so fast. Anyway, was sent to me by a FB friend. Some of you experts might want to look at it and see if it is valid. Seems that she is suggesting Diamox as a treatment:
This is Diamox:

Acetazolamide - Wikipedia
en.wikipedia.org
I’ve had a look into this and found this article: Source
Note that it was put into the peer-review process on the 7th of March 2020 and accepted for publication on the 20th of March 2020. I’ve highlighted the relevant passages.
Acetazolamide, Nifedipine and Phosphodiesterase Inhibitors: Rationale for Their Utilization as Adjunctive Countermeasures in the Treatment of Coronavirus Disease 2019 (COVID-19)
Isaac Solaimanzadeh
Published: March 20, 2020 (see history)
DOI: 10.7759/cureus.7343
Cite this article as: Solaimanzadeh I (March 20, 2020) Acetazolamide, Nifedipine and Phosphodiesterase Inhibitors: Rationale for Their Utilization as Adjunctive Countermeasures in the Treatment of Coronavirus Disease 2019 (COVID-19). Cureus 12(3): e7343. doi:10.7759/cureus.7343
Abstract
Effective treatments for Coronavirus Disease 2019 (COVID-19) outbreak are urgently needed. While anti-viral approaches and vaccines are being considered immediate countermeasures are unavailable. The aim of this article is to outline a perspective on the pathophysiology of COVID-19 in the context of the currently available clinical data published in the literature. This article appreciates clinical data published on COVID-19 in the context of another respiratory illness - high altitude pulmonary edema (HAPE). Both conditions have significant similarities that portend pathophysiologic trajectories. Following this potential treatment options emerge.
Both COVID-19 and HAPE exhibit a decreased ratio of arterial oxygen partial pressure to fractional inspired oxygen with concomitant hypoxia and tachypnea. There also appears to be a tendency for low carbon dioxide levels in both as well. Radiologic findings of ground glass opacities are present in up to 86% of patients with COVID-19 in addition to patchy infiltrates. Patients with HAPE also exhibit patchy infiltrates throughout the pulmonary fields, often in an asymmetric pattern and CT findings reveal increased lung markings and ground glass-like changes as well. Widespread ground-glass opacities are most commonly a manifestation of hydrostatic pulmonary edema. Similarly, elevated fibrinogen levels in both conditions are likely an epiphenomenon of edema formation rather than coagulation activation. Autopsy results of a COVID-19 fatality revealed bilateral diffuse alveolar damage associated with pulmonary edema, pro-inflammatory concentrates, and indications of early-phase acute respiratory distress syndrome (ARDS). HAPE itself is initially caused by an increase in pulmonary capillary pressure and induces altered alveolar-capillary permeability via high pulmonary artery hydrostatic pressures that lead to a protein-rich and mildly hemorrhagic edema. It appears that COVID-19 and HAPE both discretely converge on ARDS. In light of this, a countermeasure that has been shown to be effective in the analogous condition of HAPE is Acetazolamide. Acetazolamide has a myriad of effects on different organ systems, potently reduces hypoxic pulmonary vasoconstriction, improves minute ventilation and expired vital capacity. Other therapeutics to consider that are also directed towards decreased pulmonary pressure include Nifedipine and Phosphodiesterase inhibitors.
This review describes COVID-19 in parallel to HAPE. Deranged respiratory parameters that are present in both conditions are highlighted. The utilization of medications found to be effective in HAPE, for the treatment of COVID-19, is proposed. Given the medical emergency of a growing contagion and the thousands of lives at stake, expedient attempts to improve survival are needed. Acetazolamide, Nifedipine and Phosphodiesterase inhibitors may be potential countermeasures.
Introduction & Background
Effective treatments for Coronavirus Disease 2019 (COVID-19) outbreak are urgently needed. While anti-viral approaches are being considered and trials as well as vaccines may be forthcoming, immediate countermeasures are still remiss [1].
In ideal circumstances medications are intentionally designed, profiled and tested to combat initiators of pathophysiologic processes. However, when that is not available, there may be a need to consider treatment regimens from analogous disease patterns. Matching clinical dispositions can be considered in efforts to develop therapeutic interventions. Moreover, dire outcomes of illness may be overcome with adjunctive measures that do not necessarily cure underlying disease. Rather, supportive care as well as adjunctive countermeasures may assist patients in surviving viral illness.
The aim of this article is to outline a perspective on the pathophysiology of COVID-19 in the context of the currently available clinical data published in the literature. Following a characterization of the disease vis-a-vis a similar respiratory illness, potential treatment options may emerge.
Review
Supportive management with specific Respiratory and Ventilator support are current mainstays of treatment [2]. Sequential progression of respiratory compromise has been observed - highlighting the primacy of respiratory malfunction in overall clinical demise [3].
Therefore, garnering management approaches from similar respiratory conditions may be beneficial. Analyzing clinical data reported in published studies reveal striking similarities to high altitude pulmonary edema (HAPE) as manifested during the acute hypoxic ventilatory response.
To begin with, in severe cases, both COVID-19 and HAPE exhibit a decreased ratio of arterial oxygen partial pressure to fractional inspired oxygen (Pao2:FiO2 ratio) with concomitant hypoxia and tachypnea [4,5]. There also appears to be a tendency for low carbon dioxide levels in COVID-19 as the median partial pressure of carbon dioxide (PaCO2) level was 34 mmHg (inter-quartile range: 30-38; normal range: 35-48) in a recent JAMA article describing 138 hospitalized cases [6]. Initial exposure to hypoxia at high altitude leads to an immediate increase in ventilation that blows off large quantities of carbon dioxide, producing hypocapnia as well [7]. Furthermore, blood gases of non-acclimatized mountaineers with severe illness were accompanied by a significant decrease in arterial oxygen due to an increase in alveolar-arterial oxygen difference, although herein arterial PaCO2 did not change significantly [8]. In short, hypoxia and hypocapnia are seen in both conditions, but there is more.
Radiologic findings of ground-glass opacities are present in up to 86% of patients with COVID-19 with 76% having bilateral distribution and 33% peripheral [9]. Notably, lung cavitations, discrete pulmonary nodules, pleural effusions, and lymphadenopathy were absent [10]. In addition to this, patchy infiltrates are present [11]. Patients with HAPE also exhibit patchy infiltrates throughout the pulmonary fields, often in an asymmetric pattern and CT findings reveal increased lung markings and ground glass-like changes as well [12-14]. It has been shown that widespread ground-glass opacities are most commonly a manifestation of hydrostatic pulmonary edema and this is a central point to consider going forward [15].
See, all older patients in a familial cluster had elevated fibrinogen levels [16]. In tandem, markers of fibrin formation were significantly elevated in HAPE and Fibrin generation in that condition is deliberated as an epiphenomenon of edema formation rather than coagulation activation [8]. Altogether, these specific pulmonary clinical manifestations exhibit identical features between both COVID-19 and HAPE.
There certainly is much to ascertain with regard to the precise pathophysiology of COVID-19. Investigation of virulent properties of COVID-19 as well inflammatory responses and their effects on Alveolar integrity requires further study. Autopsy results of a COVID-19 fatality revealed bilateral diffuse alveolar damage associated with pulmonary edema, pro-inflammatory concentrates, and indications of early-phase acute respiratory distress syndrome (ARDS) [17]. HAPE itself is initially caused by an increase in pulmonary capillary pressure [18]. HAPE induces altered alveolar-capillary permeability via high pulmonary artery hydrostatic pressures that lead to a protein-rich and mildly hemorrhagic edema [19]. COVID-19 and HAPE both discretely converge on ARDS [5,17].
Yet, it can be posited that beginning early treatment may prevent ARDS development. Regardless of pathophysiologic triggers, stark clinical endpoints are apparent and similar in nature. Ultimately, distinctive pulmonary specific parameters in severe disease have comparable patterns (Table 1).
Table 1: Similar patterns of pulmonary disease between HAPE and COVID-19
Parameter HAPE COVID-19 Pao2:FiO2 ratio Decreased Decreased Hypoxia Present Present Tachypnea Increased Increased PaCO2 level Decreased Decreased Ground Glass Opacities on Chest CT Present Present Patchy Infiltrates on Chest X-RAY Present Present Fibrinogen levels/Fibrin formation Increased Increased Alveolar compromise Present Present Acute Respiratory Distress Syndrome Development in Severe Disease Present Present
HAPE: High altitude pulmonary edema; COVID-19: Coronavirus disease 2019; Pao2:FiO2 ratio: Arterial oxygen partial pressure to fractional inspired oxygen ratio; PaCO2 level: Partial pressure of carbon dioxide; Chest CT: Computed tomography of chest.
In light of this, a countermeasure that has been shown to be effective in high altitude illness is Acetazolamide.
Acetazolamide has a myriad of effects on different organ systems [20]. It potently reduces hypoxic pulmonary vasoconstriction [21]. Improved minute ventilation and expired vital capacity has been shown in climbers taking Acetazolamide as well [22].
Furthermore, over 70% of patients with COVID-19 had elevated lactate dehydrogenase levels [23]; this too may be connected to hypoxia. Evidently, Acetazolamide has physiologic effects that delay plasma lactate appearance with no effect on ventilatory threshold [24].
Other therapeutics that have been shown to be effective in the analogous condition of HAPE and that are directed towards decreased pulmonary pressure include Nifedipine and Phosphodiesterase inhibitors (Table 2) [25,26].
Table 2: Sample medications and dosages utilized in high altitude illness and HAPE
Acetazolamide 250 mg every 12 hours Nifedipine 30 mg extended release every 12 hours Sildenafil 20-50 mg every 8 hours Tadalafil 10 mg every 12 hours
HAPE: High altitude pulmonary edema
Conclusions
This review describes COVID-19 in parallel to HAPE. Deranged respiratory parameters that are present in both conditions are highlighted. The utilization of medications found to be effective in HAPE for the treatment of COVID-19 is proposed. Given the medical emergency of a growing contagion and the thousands of lives at stake, expedient attempts to improve survival are needed. Acetazolamide, Nifedipine and Phosphodiesterase inhibitors may present an opportunity for countermeasure development.
References
- Li G, De Clercq E: Therapeutic options for the 2019 novel coronavirus (2019-nCoV). Nat Rev Drug Discov. 2020, 19:149-150. 10.1038/d41573-020-00016-0
- Arabi YM, Fowler R, Hayden FG: Critical care management of adults with community-acquired severe respiratory viral infection. Intensive Care Med. 2020, 46:315-328. 10.1007/s00134-020-05943-5
- Huang C, Wang Y, Li X, et al.: Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020, 395:497-506. 10.1016/S0140-6736(20)30183-5
- Wang M, Zhou Y, Zong Z, et al.: A precision medicine approach to managing 2019 novel coronavirus pneumonia. Precis Clin Med. 2020, pbaa002:10.1093/pcmedi/pbaa002
- Ma SQ, Wu TY, Cheng Q, Li P, Bian H: Acute respiratory distress syndrome secondary to high-altitude pulmonary edema: a diagnostic study. J Med Lab Diagn. 2013, 4:1-7. 10.5897/JMLD12.007
- Wang D, Hu B, Hu C, et al.: Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020, 323:1061-1069. 10.1001/jama.2020.1585
- Taylor AT: High-altitude illnesses: physiology, risk factors, prevention and treatment. Rambam Maimonides Med J. 2011, 2:e0022. 10.5041/RMMJ.10022
- Bartsch PE, Waber U, Haeberli AN, Maggiorini M, Kriemler S, Oelz O, Straub WP: Enhanced fibrin formation in high-altitude pulmonary edema. J Appl Physiol. 1987, 63:752-757. 10.1152/jappl.1987.63.2.752
- Kanne JP: Chest CT findings in 2019 novel coronavirus (2019-nCoV) infections from Wuhan, China: key points for the radiologist. Radiology. 2020, 295:200241. 10.1148/radiol.2020200241
- Chung M, Bernheim A, Mei X, et al.: CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology. 2020, 295:200230. 10.1148/radiol.2020200230
- Pan Y, Guan H, Zhou S, et al.: Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. (Epub ahead of print). Eur Radiol. 2020, 10.1007/s00330-020-06731-x
- Kobayashi T, Koyama S, Kubo K, Fukushima M, Kusama S: Clinical features of patients with high-altitude pulmonary edema in Japan. Chest. 1987, 92:814-821. 10.1378/chest.92.5.814
- Bärtsch P, Swenson ER, Maggiorini M: Update: high altitude pulmonary edema. Adv Exp Med Biol. 2001, 502:89-106. 10.1007/978-1-4757-3401-0_8
- Zhou Q: Standardization of methods for early diagnosis and on-site treatment of high-altitude pulmonary edema. Pulm Med. 2011, 2011:7. 10.1155/2011/190648
- Hewitt MG, Miller WT Jr, Reilly TJ, Simpson S: The relative frequencies of causes of widespread ground-glass opacity: a retrospective cohort. Eur J Radiol. 2014, 83:1970-1976. 10.1016/j.ejrad.2014.06.025
- Chan JF, Yuan S, Kok KH, et al.: A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020, 395:514-523. 10.1016/S0140-6736(20)30154-9
- Xu Z, Shi L, Wang Y, et al.: Pathological findings of COVID-19 associated with acute respiratory distress syndrome. (Epub ahead of print). Lancet Respir Med. 2020, 10.1016/S2213-2600(20)30076-X
- Maggiorini M, Mélot C, Pierre S, et al.: High-altitude pulmonary edema is initially caused by an increase in capillary pressure. Circulation. 2001, 103:2078-2083. 10.1161/01.CIR.103.16.2078
- Swenson ER, Maggiorini M, Mongovin S, Gibbs JSR, Greve I, Mairbäurl H, Bärtsch P: Pathogenesis of high-altitude pulmonary edema: inflammation is not an etiologic factor. JAMA. 2002, 287:2228-2235. 10.1001/jama.287.17.2228
- Leaf DE, Goldfarb DS: Mechanisms of action of acetazolamide in the prophylaxis and treatment of acute mountain sickness. J Appl Physiol. 2007, 102:1313-1322. 10.1152/japplphysiol.01572.2005
- Swenson ER: Carbonic anhydrase inhibitors and hypoxic pulmonary vasoconstriction. Respir Physiol Neurobiol. 2006, 151:209-216. 10.1016/j.resp.2005.10.011
- Larson EB, Roach RC, Schoene RB, Hornbein TF: Acute mountain sickness and acetazolamide: clinical efficacy and effect on ventilation. JAMA. 1982, 248:328-332. 10.1001/jama.1982.03330030034021
- Chen N, Zhou M, Dong X, et al.: Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020, 395:507-513. 10.1016/S0140-6736(20)30211-7
- Scheuermann BW, Kowalchuk JM, Paterson DH, Cunningham DA: Carbonic anhydrase inhibition delays plasma lactate appearance with no effect on ventilatory threshold. J Appl Physiol. 2000, 88:713-721. 10.1152/jappl.2000.88.2.713
- Bartsch P, Maggiorini M, Ritter M, Noti C, Vock P, Oelz O: Prevention of high-altitude pulmonary edema by nifedipine. N Engl J Med. 1991, 325:1284-1289. 10.1056/NEJM199110313251805
- Maggiorini M: Prevention and treatment of high-altitude pulmonary edema. Prog Cardiovasc Dis. 2010, 52:500-506. 10.1016/j.pcad.2010.03.001
To sum up the finings (and thus the rationale behind using Acetazolamide in the treatment of the pulmonary aspects of Covid-19 infection:
- Deaths from Covid-19 are mostly related to a breakdown of oxygenation of the blood in the lung
- This is the same in High-altitude pulmonary edema (HAPE)
- Severe Covid-19 infection and HAPE share other clinical findings
- Acetazolamide is a proven therapeutic measure in HAPE, probably mostly by reducing vasoconstriction of the vessels in the lung
- Hence the idea that Acetazolamide might be effective in treating pulmonary complications of a COVID-19 infection.
The whole thing makes sense to me - HOWEVER, as so often happens in medicine, a once logical idea turned out to be completely useless or detrimental once it was rigorously tested (like beta-blockers in heart failure, or activated protein VII in sepsis etc).
Acetazolamide in itself is a medication that has been around for a long time. It is cheap and it’s side-effects profile is well-known. So I think it would be worth trying out the drug in severe cases that haven’t progressed to respiratory failure yet.
A word of caution: While acetazolamide itself doesn’t have any effect on the QT-interval (in the ECG), it can worsen your potassium levels (which can prolong QT). Hydroxychloroquine can prolong the QT-interval, so any concomitant use of the two drugs should be carefully monitored (by ECG and potassium levels).
Hope that makes sense!
This is from a discussion with a friend who is a mortuary driver:
While preparing the body of a very elderly woman for transport, the nurse in attendance said that she'd died from cardiac arrest. When he collected the death certificate, it said cause of death COVID-19.
He further commented:
"Hospital staff, regardless of what they know, tend to prefer to keep their mouths shut....keep their jobs, pay their mortgages. Very few humans are courageous."
With the above in mind and apart from the above, I have 14 peeps amongst friends and family outside of this network who work in medical professions or attached care industries: ambulance/paramedic, registered nurses, ordinary nurses, pathology collection, aged/disability care, administration.
One has gone full nazi - promotes the dobber hotline, posts about staying indoors to save lives etc. She also posts updated statistics for her state and as of yesterday the death toll was 7.
Some of the others seemed behind the lockdown measures initially but have gone strangely silent since then. One registered nurse likes the odd post that I put up and made a comment 'I agree, it's all BS'.
A hospital midwife initially posted video's of herself talking about the lockdowns and encouraging peeps to comply. It seems she has since been put off work and now posts about stay at home activities.
My niece, an NICU nurse is all in to protect the fragile babies. She is young and has only worked this job for about year after qualifying. Though one would have thought that the hospital would have already had procedures in place to prevent babies catching viruses under ordinary circumstances.
I'm thinking that there could be plenty more who see what is going on from the perspective of various industries and endeavours and don't feel as though they are in a position to talk about it for whatever reason. Despite accepting the idea that there are those who won't wake up, those who are but are not in the position to speak out might take some comfort from that fact that there are those who are speaking out.
While preparing the body of a very elderly woman for transport, the nurse in attendance said that she'd died from cardiac arrest. When he collected the death certificate, it said cause of death COVID-19.
He further commented:
"Hospital staff, regardless of what they know, tend to prefer to keep their mouths shut....keep their jobs, pay their mortgages. Very few humans are courageous."
With the above in mind and apart from the above, I have 14 peeps amongst friends and family outside of this network who work in medical professions or attached care industries: ambulance/paramedic, registered nurses, ordinary nurses, pathology collection, aged/disability care, administration.
One has gone full nazi - promotes the dobber hotline, posts about staying indoors to save lives etc. She also posts updated statistics for her state and as of yesterday the death toll was 7.
Some of the others seemed behind the lockdown measures initially but have gone strangely silent since then. One registered nurse likes the odd post that I put up and made a comment 'I agree, it's all BS'.
A hospital midwife initially posted video's of herself talking about the lockdowns and encouraging peeps to comply. It seems she has since been put off work and now posts about stay at home activities.
My niece, an NICU nurse is all in to protect the fragile babies. She is young and has only worked this job for about year after qualifying. Though one would have thought that the hospital would have already had procedures in place to prevent babies catching viruses under ordinary circumstances.
I'm thinking that there could be plenty more who see what is going on from the perspective of various industries and endeavours and don't feel as though they are in a position to talk about it for whatever reason. Despite accepting the idea that there are those who won't wake up, those who are but are not in the position to speak out might take some comfort from that fact that there are those who are speaking out.
I found some more numbers. The bad news is that this pandemic does seem to be real in Western Europe, but mostly for elderly, because the overall mortality is higher than in previous years. You can find graphs for Netherlands and Spain in below links. Here are the percentages for deaths:
It's hard to keep up with this thread, so perhaps this has already been mentioned/discussed, fwiw.
According to The Guardian:
Half of coronavirus deaths happen in care homes, data from EU suggests
Figures from Italy, Spain, France, Ireland and Belgium suggest UK may be underestimating care sector deaths.
If true, it means that about a half of coronavirus deaths in Europe were the elderly people who died without proper medical care, they were not hospitalized.
This is a very good find Ellipse.Its nice to hear these information from Eisenhower GGD.Very powerful indeed.On a more esoteric touch, I found this video of Laura Eisenhower, great-granddaughter of Eisenhower, interesting.
There's a bit of "light forces will save us" into it, but I was surprised by her good overall perception of what is happening.
fwiw
She nailed it about the vampires feeding on our stress.This is a very good find Ellipse.Its nice to hear these information from Eisenhower GGD.Very powerful indeed.
I´m still behing with the thread, but Im receiving a news from Italian friend about that France found out traces of the virus in the water . non potable water, here is the link so I think is best to check this, this is crazy.
Traces of coronavirus found in water in France
Traces of coronavirus found in water in France
Traces of coronavirus found in water in France
Traces of coronavirus found in water in France
Traces of the novel coronavirus have been discovered in the non-potablee water supply in the French capital of Paris, news agency AFP reported, while quoting officials who reassured that the drinking water supply was "fine". According to the report, the Paris water authority's laboratory detected tiny amounts of the virus in four of 27 samples collected from around the capital, and the network was shut down as precaution. The non-potable water is usually used from networks like the Seine river for gardening and other activities. "Drinking water is supplied from a totally independent network and can be consumed without any risk," said Blauel, the city's top environmental official.
France's prime minister said the country was starting to beat back the coronavirus as the outbreak's death toll approached 20,000 Sunday while new hospitalisations continued a slow decline. The country reported 395 deaths from COVID-19 in the last 24 hours, the government said, bringing the epidemic tally to 19,718. But in a positive sign, the number of people in hospital declined for the fifth day in a row to 30,610, a small decline of 29, top health official Jerome Salomon told a televised press conference. There were 5,744 people in intensive care, added Salomon, 89 fewer in the 11th consecutive day of decline. "We are scoring points against the epidemic," Prime Minister Edouard Philippe told the same briefing, adding the "situation is improving gradually, slowly, but surely" and the epidemic is "slowing". But he stressed that a nationwide lockdown which entered into force on March 17 to halt the spread of the virus must be strictly respected until May 11, when it will start being lifted in phases.
Ads by optAd360
France expects its worse recession in 2020 since the end of World War II, with economic activity down 36 percent since the lockdown started. But economic life cannot resume until the virus has stopped circulating among the population and hospitals' capacity to treat the seriously ill is restored, the prime minister said.
-Inputs from agencies
TAGS
I think they key thing about NZ is that “they” desperately need this country as a bunker. Billionaires have been buying bunkers here for the past several years. They desperately want control of this population so the programming has been the most intense here.It is a really interesting question. I'm not sure I have an answer. Maybe because we are at the literal end of the world, so far away form any other country (other than Australia). The reaction to CV1984 is just so disproportionate to the actual results it is gobsmacking. Today there was an article in the press by the Deputy PM - different party to the PM as the government is a coalition. He said we need to get the economy back up and running, even just to make sure there is still the ability to deliver essential services. The attacks on him have been horrendous.
The academics that are advising the priminister all seem to have some kind of connection to the WHO. Present or in the past.
So they have come down really hard here.
And of course everyone thinks Jacinda Ardern is a saint, never mind she is an inexperienced and naive puppet.
Ketone Cop
Jedi Council Member
Thanks, I downloaded it. I will try to edit my post there and see what it can do. When I do get it done, where does someone submit articles for consideration by SOTT?
I feel another one coming in my continuing ruminations as I consider Seamas' reply to my post on Naessens. I think it is important, because if what Gaston Naessens and the others saw in their work is true, then not only does the terrain (e.g. the condition of the body or environment) matter, but:
The "terrain" determines the DNA that manifests therein.
What Naessens, Rife, Reich, and Bechamp may have witnessed with their advanced microscopes is analogous to the discoveries that Antonie van Leeuwenhoek and Galileo Galilei made with the inventions of the first microscope and telescopes, respectively.
As Leeuwenhoek and Galileo expanded the 3D vision of man beyond the accepted limits of reality during their times; so, too, have these four men done so with their advanced light microscope technologies (each of whom developed similar instruments independently of one another, over 100 years apart in time) which allowed them to visualize living organisms at magnifications only reportedly possible by electron microscopes. In fact: if the work that they did, independently of each other yet with very similar results, repeatedly - is confirmed, then:
what they were witnessing is nothing less than intelligent design in action.
No WONDER their discoveries were dealt with so harshly by the medical complex of their times! What they discovered threatened to expose their backwards "health" system. Three of these men had their careers ruined; one (Bechamp) was almost forgotten to history though his discoveries were at least as great as Pasteur; and two of them were prosecuted for their work, with Reich dying in prison - after which all of his work was seized and destroyed (six tons of it) by the government and his name forever sullied afterwards.
I think this forum is ready now for this information, after the Behe material. If anyone wants to get a jump on this stuff, I thank Channa for this gem of a find - a FREE download of Christopher Bird's book:
I saw her message more as a message to the universe than to the the forces ruling, for sure. And the "We do not consent" just one in the right direction.She really has, but on the other hand she doesn't seem to realize the nature of psychopaths. She probably considers the cabal members as souls with a negative polarization.
"You're going too far," she says. That will only earn her a wry smile from the entities she's trying to address.
I like her mentioning the power of cosmic and natural law, the only authority that the PTB will eventually have to accept.
"We do not consent." Doesn't the majority on this planet still consent?
And finally: "We're not your experiments!" I remember the C's mentioning that humanity is indeed an experiment but
not by 4D-STS alone.
About the experience, I want to believe there is different levels involved. I would say, on a upper level, we are an experience in term of free will. On a lesser level, in term of invasion. So to stand up and say "We're not your experiments!" is a good thing because it send a message in the right direction and raise the level of consciousness which is the start point of a real protection, i.e. knowledge protect.
And from this point of consciousness, you can take actions in the 3D world: protecting yourself, spreading the word, and so on...
Last edited:
Sol Logos
The Living Force
Donald Trump as President isn't very believable
Oh it definitely gets weirder!
Our favorite 'spirit cooker' doing art collaborations with Microsoft
"mixed reality"
Here's another odd Microsoft thing. It's a patent that recently came out: WO2020060606 CRYPTOCURRENCY SYSTEM USING BODY ACTIVITY DATA
Of course the patent number has 666 in it. What else could we expect?
WO2020060606 - CRYPTOCURRENCY SYSTEM USING BODY ACTIVITY DATA
Abstract:
Human body activity associated with a task provided to a user may be used in a mining process of a cryptocurrency system. A server may provide a task to a device of a user which is communicatively coupled to the server. A sensor communicatively coupled to or comprised in the device of the user may sense body activity of the user. Body activity data may be generated based on the sensed body activity of the user. The cryptocurrency system communicatively coupled to the device of the user may verify if the body activity data satisfies one or more conditions set by the cryptocurrency system, and award cryptocurrency to the user whose body activity data is verified.
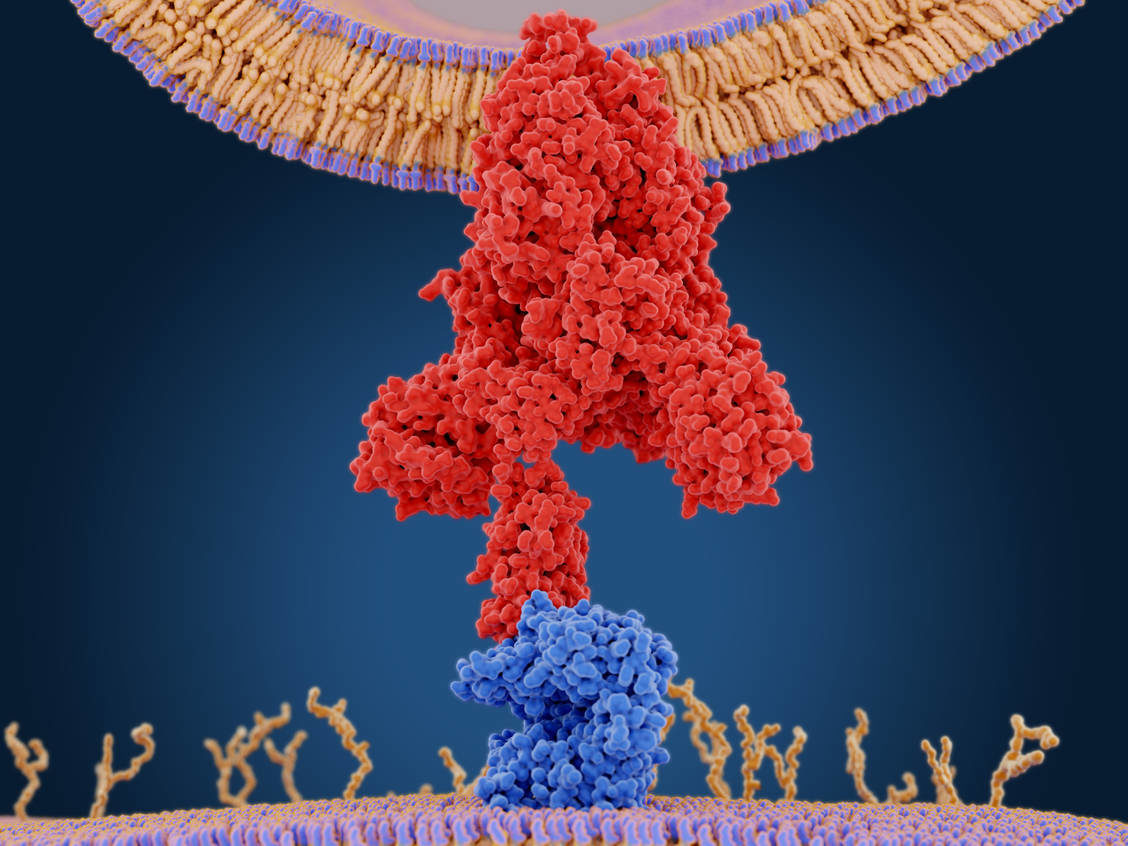
Fascinating article posted over at SOTT.net that has focus on ACE2 proteins, the autonomic nervous system, and equally while looking into the parasympathetic system. Gaby could point things out further, yet there are two studies concerning Nicotine receptors seen through the lens of both pro and con, and what the con side seems to have missed relating to their findings.
Nice work!
 www.sott.net
www.sott.net
Nice work!
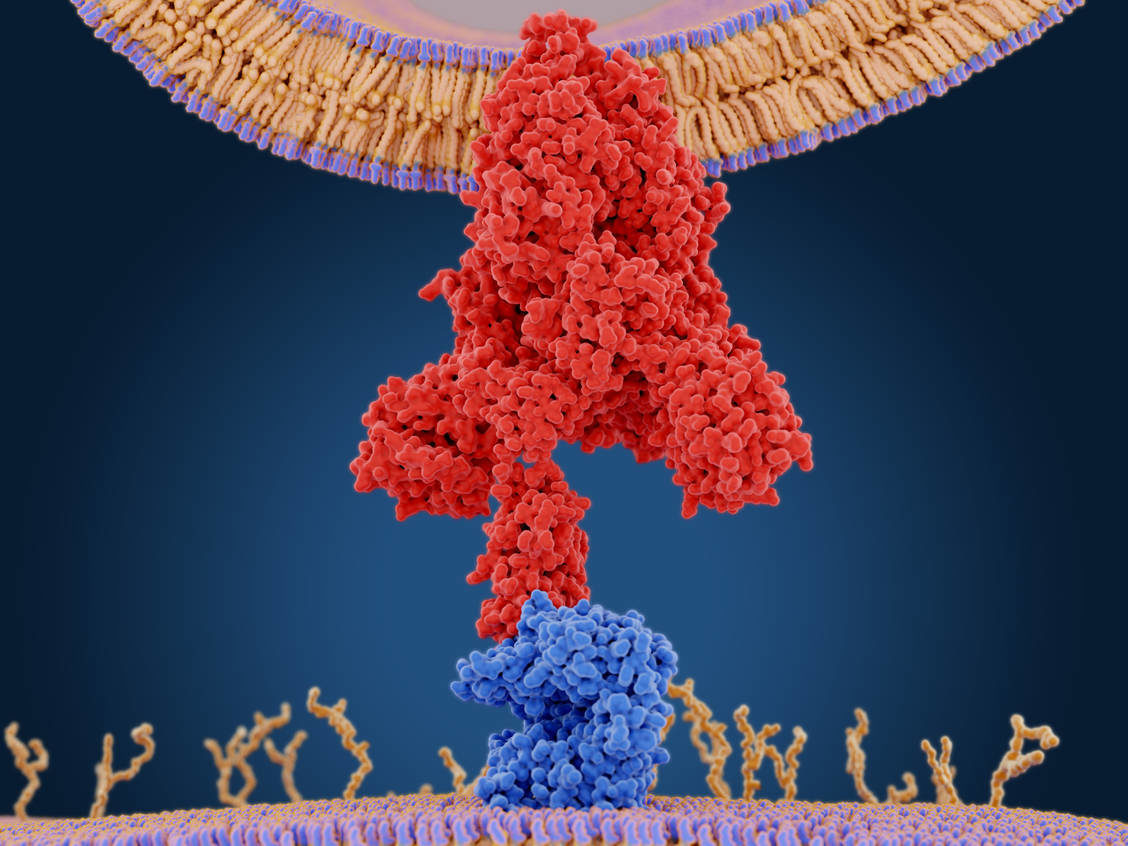
COVID-19, ACE2, Nicotinic Receptors And The Cholinergic Anti-Inflammatory And Cognitive-Improving Pathway
I've been reading case reports of heart damage in people infected with COVID-19. In fact, someone in my close circle had an episode of fulminant myopericarditis and a strange lung pathology last December, from which he miraculously recovered. I...
TheSpoon
Jedi
It's not "in advance" if your associates have access to time travel (which need be no more than messaging). A "knee jerk reaction" could appear 100 years in the past.Also, one wonders if the "anti-tobacco" campaign was instigated for this very reason? That is, were they planning that far in advance?
Taiwan has open businesses and schools, pro baseball playing, no shutdowns, and the result is 6 deaths and 400 infections out of a population of 23 million.
Taiwan's Vice-President Chen Chien-jen on his country's fight with Covid-19
The leading epidemiologist explains how Taiwan's long-planned response has so far contained the virus
By Nicola Smith, Asia correspondent, Taipei 18 April 2020 • 9:30pm
Taiwan’s reaction to Covid-19 has been fast and effective. Despite its proximity to China, it has seen just 395 cases and six deaths. In an exclusive interview, Chen Chien-jen, the country’s vice-President and renowned epidemiologist, explains Taiwan’s coronavirus battleplan and the lessons it holds for Britain and the WHO. Answers have been edited for space.
What did Taiwan learn from Sars in 2003?
We learned a lot about prudent action, rapid response and early deployment.
It’s important to monitor emerging infectious diseases, especially in this region because we are near to China. In addition to SARS, there was an H1N1 Avian Flu in 2005, an H7N9 Avian Flu and now Covid-19.
Secondly, we announce a travel alert if necessary and thirdly, we optimize border quarantine to identify imported cases. This time when we knew there was an atypical pneumonia – meaning an infectious lung disease without known cause, where the patient is isolated and there is likely human-to-human transmission – we implemented on-board quarantine for all passengers flying from Wuhan.
Then there is 14-day home quarantine for close contacts of passengers from affected areas. During SARS we found that hospital-acquired infection was very dangerous so we upgraded the healthcare system to provide isolation rooms and a national network of health care centres for infectious diseases. This strategy has to be planned before an outbreak.
An adequate supply of PPE is important. In 2002, we ran short of N95 face masks so we knew we needed a face mask rationing system and to increase production. We now produce more than 13 million a day and are expecting to push this up to 15m.
Then there’s health education about home quarantine or what children have to do at school. This and risk communication must be transparent.
How many critical care beds do you have?
At full capacity, we have 20,000 isolation rooms, and 14,000 ventilators.
We also set up a National Epidemic Command Centre because outbreak control is an inter-ministerial effort and it is essential to coordinate. It’s very important that everyone in the country has to be involved - the government and the people.
Can Taiwan’s pandemic strategy be successfully replicated in bigger countries? Can lessons still be learned?
Yes, sure. It will never be too late to control any kind of outbreak in any country. There are still a lot of chances for different countries to adopt good strategies developed here to help contain the outbreak. Social distancing and good health behaviour are definitely important – frequent handwashing, measuring body temperature, using a face mask if necessary. At home, close contacts [of the infected] shouldn’t dine together. The [patient] can live in a single room. It’s not necessary to stop all activities. As long as more than 50% of the population reduces 50% of their social contacts then the outbreak can be controlled. They can go to school, to work but must reduce non-essential recreation and social contact.
Home quarantine is important. Close contacts must stay at home for 14 days and check their health status.
Frontline healthcare workers must have adequate PPE. The UK and US are trying their best to do that and Taiwan is willing to help.
We need to collaborate to develop rapid diagnostics, anti-virals or even vaccines as soon as possible.
What recommendations do you have for the UK? Could mass testing help?
In Taiwan we didn’t practice mass testing because among 395 cases, only 55 were locally transmitted, and the infection source could not be traced in only ten cases. If many cases have no known infection sources then you have to do mass testing. But it is sometimes neither efficient nor cost effective. You have to test [patients’] close contacts as a first priority, then high-risk groups – healthcare workers, supermarket cashiers, taxi and public transport drivers. If they aren’t infected then others won’t be.
Western pandemic planning documents don’t envisage the lockdowns we’re seeing in Europe or the US. Why?
Asian countries are always in greater danger of emerging infectious disease. We face a biological timebomb, so we are well-prepared. Vietnam, Singapore, Hong Kong were severely affected by Sars. That’s why they are now also doing a very good job. In Korea they had Mers so they learned from it. We are in a much more dangerous situation than America and Europe and people always learn from disasters. Our world is getting smaller so we have to share information transparently and rapidly. This is the mission of the World Health Organisation.
After Sars the WHO set up an alert system – Public Health Emergency of International Concern. When there was an H1N1 new influenza in 2009, they announced the PHEIC around one month after the first case, when only three countries were affected. So we developed rapid diagnosis, prepared anti-virals, and developed the vaccine very quickly. For Covid-19, some say the first case was in early or mid-December 2019, but this time the PHEIC was announced at the end of January. Even worse, they still did not consider any kind of travel alert. Then why announce that it’s a PHEIC? 19 countries were already affected with more than 8,000 confirmed cases, so it was too late.
Why was the WHO’s response different to Covid-19? What has been the impact of Taiwan’s exclusion from the WHO?
I don’t know why the WHO did not take actions as quickly as they did for H1N1 or Sars. The WHO didn’t invite us to an emergency meeting on 22-23 January. Before that we already requested China’s CDC to send our two experts to Wuhan to look at the situation. Based on [their] observation and personal dialogue we found the situation was quite severe already in mid-January. They were discussing about whether to isolate the whole of Wuhan or not. The situation in the hospitals was really worse. We also discovered something very important – they were paying much more attention to hospitalised severe cases. When we asked about close contact tracing and the care of patients with mild symptoms, we didn’t get a very good response. If close contact tracing can be done then the disease won’t be spread by the patient.
What do you think of China’s response to this pandemic?
Wuhan’s frontline health workers were doing a very good job taking care of the severe cases of atypical pneumonia with unknown causes. They also tried their best to share the information with the Wuhan health authorities. I don’t know why this information was not taken very seriously. Usually epidemiologists or infectious diseases physicians consider that once there is a cluster of patients in hospitals this only represents the tip of the iceberg so there must be a lot of infected people. That’s why some doctors in Wuhan shared this warning to their colleagues but unfortunately it was not taken very seriously.
Do you think there was a political cover-up?
I really don’t know but if we compare it to the alert [from] the healthcare workers, I think that the alert did not get sent out to the public or to the entire world.
You said your CDC saw a notice from Wuhan on social media on December 31 and already the Chinese CDC and the WHO. What did that notice say?
The notice said there are seven cases of atypical pneumonia but it was not considered to be SARS and the specimen has been tested for possible causes. However, all these patients were isolated for treatment.
Do you believe the virus originated in a market?
They say that the virus originated from Huanan seafood market but if we look at the first 42 cases published in academic journals, around ten have no history of going there. This is a very important hint that the market may not be the origin of this infection. In early December, there were cases reported from Thailand, Hong Kong, and Japan – all patients who did not go to the market. There might be a cluster there but not all got the infection there. From an epidemiological viewpoint, once there is a patient or a cluster you have to find their contacts and then trace two things – infection sources and whether surrounding people have been infected. But they never paid attention to mild or asymptomatic cases.
Is there any indication of where the virus came from?
When we try to trace back to the [index] case it is very difficult. If the case had a mild disease you can never find it. And according to this so-called infection pyramid of Covid-19, there is only a small proportion of severe but a lot of mild and asymptomatic cases. So for Covid-19 it is much more difficult than for Sars to identify the index case.
What is the right exit strategy for the lockdowns?
Covid-19 is becoming flu-like. It means that since it is highly contagious with many mild or asymptomatic cases, and can be transmitted through droplets and contaminated areas, we won’t get rid of this virus totally. We need to develop rapid diagnostics and anti-virals then milder cases can be treated by private practitioners in the community. Severe cases can be treated in medical centres, also with rapid diagnosis and anti-virals. This will protect and cure the patient and protect close contacts from infection. In one or 1.5 years we may have the vaccine. Before that, we need to keep social distancing…living in a self-limited way but still semi-normally.
How do we open up travel and trade again?
To coordinate international transportation, all nations have to share data and make their outbreak status transparent. We need seroepidemiological studies to test blood samples to know the infection status of each country.
What is Taiwan’s contribution to diagnostics and vaccines?
We have three vaccine development teams in collaboration with the EU and US – Academia Sinica, the National Health Research Institute, and Medigen along with the US NIH.
There are two prototype rapid diagnostics. One to test antigens. Another to test the blood – the seromarkers – to test antibodies. We hope to soon get a licence and we’re happy to share all our new developments. On pharmaceuticals, we are involved in a clinical trial of Remdesivir, which seems quite good for severe but even better for milder cases.
Will life return to normal soon?
I once gave a prediction about the end of May, but it’s very difficult to predict accurately. Europe has reached the peak and it’s going down. In the US it’s still going up. All nations have mobilised and they are doing much better than one month ago. It’s a good phenomenon of globalisation, of Covid-19 containment.
Trending content
-
-
Thread 'Coronavirus Pandemic: Apocalypse Now! Or exaggerated scare story?'
- wanderingthomas
Replies: 30K -

 The irony here is that in his first response he said, “Fact is Covid-19 is so infectious, we will allget herd immunity regardless of any lockdown or not.” So in his hysteria he failed to see he made the argument against his own position.
The irony here is that in his first response he said, “Fact is Covid-19 is so infectious, we will allget herd immunity regardless of any lockdown or not.” So in his hysteria he failed to see he made the argument against his own position.