We need to cut the crap about CO2 and begin to realize that our life and health depend on enough levels of CO2 in the blood and tissues. Carbon dioxide is a nutrient as well as a product of respiration and energy production in the cells and its lack or deficiency is of itself a starting point for different disturbances in the body.
Carbon dioxide has many protective functions including increasing Krebs cycle activity, which is the key to health and the greatest way of avoiding cancer, which happens when Krebs cycle activity slows down in the mitochondria, so fermentation has to make up the difference. Importantly, CO2 also inhibits toxic damage to proteins.
Carbon dioxide is a harmless, colourless, non-toxic, natural gas that is the key link in the carbon cycle of life. In the presence of a large amount of carbon dioxide, the hemoglobin molecule changes its shape slightly in a way that favors the release of oxygen.
Increasing carbon dioxide inhibits lactic acid formation thus helps control systemic acidification, which decreases oxygen utilization. CO2 has been found to lead to the better coordination of oxidation and phosphorylation and increased the phosphorylation velocity in liver mitochondria. Any way we put it CO2 is the key to oxygen, to life, to health.
“The end product of respiration is carbon dioxide, and it is an essential component of the life process. The
ability to produce and retain enough carbon dioxide is as important for longevity as the ability to conserve enough heat to allow chemical reactions to occur as needed. Carbon dioxide protects cells in many ways. By bonding to amino groups, it can inhibit the glycation of proteins during oxidative stress, and it can limit the formation of free radicals in the blood; inhibition of xanthine oxidase is one mechanism (Shibata, et al., 1998). It can reduce inflammation caused by endotoxin/LPS, by lowering the formation of tumor necrosis factor, IL-8 and other promoters of inflammation (Shimotakahara, et al., 2008). It protects mitochondria (Lavani, et al., 2007), maintaining (or even increasing) their ability to respire during stress,” writes
Dr. Ray Peat.
“The suppression of mitochondrial respiration increases the production of toxic free radicals, and the decreased carbon dioxide makes the proteins more susceptible to attack by free radicals. The presence of
carbon dioxide is an indicator of proper mitochondrial respiratory functioning. In every type of tissue, it is the failure to oxidize glucose that produces oxidative stress and cellular damage,” Dr. Peat adds, and then concludes, “A focus on correcting the respiratory defect would be relevant for all diseases and conditions (including heart disease, diabetes, dementia) involving inflammation and inappropriate excitation, not just for cancer. Carbon dioxide has a stabilizing effect on cells, preserving stem cells, limiting stress and preventing loss of function.”
Over the oxygen supply of the body carbon
dioxide spreads its protecting wings.
Friedrich Miescher
Swiss physiologist, 1885
“The German cancer researcher Dr. Paul Gerhard Seeger
[1] demonstrated in 1938 that in most cases cancer starts in the cytoplasm, the jelly-like outer part of the cell, and especially in the energy-producing mitochondria. Here food fragments are normally oxidized in a series of enzymatic steps called the ‘respiratory chain’. Seeger showed that
in cancer cells this respiratory chain was more or less blocked, especially at the site of the important enzyme cytochrome oxidase. Without it the cell can produce energy only anaerobically like a fungal cell. This is very inefficient, and the resulting overproduction of lactic acid adding even more acidity to usually an already acidic body. In 1957 Seeger also successfully transformed normal cells into cancer cells within a few days by introducing chemicals that blocked the respiratory chain.
Without enough oxygen, the electron transport chain becomes jammed with electrons. Consequently, NAD
[2] cannot be produced, thereby causing glycolysis to produce lactic acid instead of pyruvate, which is a necessary component of the Krebs Cycle.
In general, we tend to assume that cancer cells are generating energy using glycolysis rather than mitochondrial oxidative phosphorylation, and that the mitochondria were dysfunctional. Advances in research techniques have shown the mitochondria in cancer cells to be at least partially functional across a range of tumour types. However, different tumour populations have different bioenergetic alterations in order to meet their high energy requirement meaning
the Warburg effect is not consistent across all cancer types.[3] Cancer does not translate into annihilation of cells mitochondria however it does mean the cell are fermenting because of compromised oxidization.
CO2 has Antioxidant Properties
Normal arterial levels of CO2 have antioxidant properties. Indeed, a group of Russian microbiologists discovered that "CO2 at a tension close to that observed in the blood (37.0 mm Hg) and high tensions (60 or 146 mm Hg) is a potent inhibitor of generation of the active oxygen forms (free radicals) by the cells and mitochondria of the human and tissues" (Kogan et al, 1997). Dozens of studies have shown that modern "normal subjects" breathe about 12 L/min at rest, while the medical norm is only 6 L/min. As result, blood CO2 levels is less than normal.
As we have seen arterial hypocapnia (CO2 deficiency) causes tissue hypoxia that trigger numerous pathological effects. Cell hypoxia is the main cause of free radical generation and oxidative stress and CO2 deficiency in the blood is one of the main causes of hypoxia (low oxygen).
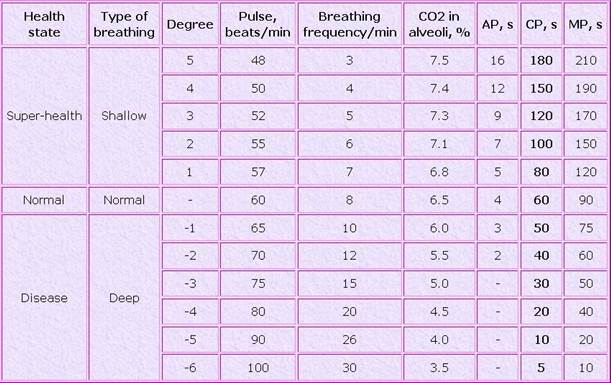
Having a normal level of CO2 in the lungs and arterial blood (40 mm Hg or about 5.3% at sea level) is imperative for normal health. Do modern people have normal CO2 levels? When reading the table below note that levels of CO2 in the lungs are inversely proportional to minute ventilation rates, in other words, the more air one breaths the lower the level of alveolar CO2.
Dr. Lynne Eldridge and many others have noted most modern adults breathe much faster (about 15-20 breaths per minute) than what would be considered a healthy respiratory rate. Respiratory rates in cancer and other severely ill patients are usually higher, generally about 20 breaths/min or more. Meaning the general population is driving down oxygen available to cells opening the door to increased incidences of cancer. Heavy metal and chemical toxification of the cells further impede oxygen with nutritional deficiencies are the slam dunk that leads to cancer.
Oxygen availability to cells decreases glucose oxidation, whereas
oxygen shortage consumes glucose faster in an attempt to produce ATP via the less efficient anaerobic glycolysis to lactate. This is much of the basis of oxygen therapy in cancer and a full range of other diseases because most chronically ill people, if not all, are having a hard time with both oxygen and its perfectly mated gas, carbon dioxide. In cancer treatment this comes with the bonus of stimulating the immune system’s cancer killer cells.
Perfectly Normal Until it's Cancer
We can take some lessons from our muscles when they are worked hard. When the body has plenty of oxygen, pyruvate is shuttled to an aerobic pathway to be further broken down for more energy. But
when oxygen is limited, the body temporarily converts pyruvate into a substance called lactate, which allows glucose breakdown—and thus energy production—to continue. Even in healthy athletic individuals, when we put the muscles to great challenges oxygen levels fall temporarily showing us what happens in cells when they are oxygen starved.
In cancer the change becomes permanent. Cancer cells will continue with fermentation of glucose and the production of lactate even in the presence of oxygen though some evidence that some cancer cells, especially young cancer cells can be reverted back to normal cells if they can be provided enough oxygen and enough opportunity to detoxify.
Lactic acid in our tissues is a cause of biological problems for many reasons principle among them is the fact that lactic acid displaces carbon dioxide. The main features of stress metabolism include increases of stress hormones, lactate, ammonia, free fatty acids, and fat synthesis, and a decrease in carbon dioxide. Lactic acid in the blood can be taken as a sign of defective respiration, since the breakdown of glucose to lactic acid increases to make up for deficient oxidative energy production.
Glucose can be metabolized into pyruvic acid, which, in the presence of oxygen, can be metabolized into carbon dioxide. Without oxygen, pyruvic acid can be converted into lactic acid. The decrease of carbon dioxide generally accompanies increased lactic acid production.
The ability of lactic acid to displace carbon dioxide is probably involved in its effects on the blood clotting system. It contributes to disseminated intravascular coagulation and consumption coagulopathy, and increases the tendency of red cells to aggregate, forming "blood sludge," and makes red cells more rigid, increasing the viscosity of blood and impairing circulation in the small vessels. (Schmid-Schönbein, 1981; Kobayashi, et al., 2001; Martin, et al., 2002; Yamazaki, et al., 2006.)
Lactate and inflammation promote each other in a vicious cycle (Kawauchi, et al., 2008).
Low thyroid leads to low production of
carbon dioxide and wastage of glucose.
Dr. Ray Peat
Carbon dioxide protects cells in many ways. By bonding to amino groups, it can inhibit the glycation of proteins during oxidative stress, and it can limit the formation of free radicals in the blood; inhibition of xanthine oxidase is one mechanism (Shibata, et al., 1998). It can reduce inflammation caused by endotoxin/LPS, by lowering the formation of tumor necrosis factor, IL-8 and other promoters of inflammation (Shimotakahara, et al., 2008). It protects mitochondria (Lavani, et al., 2007), maintaining (or even increasing) their ability to respire during stress.”
Carbon dioxide has a stabilizing effect on cells, preserving stem cells, limiting stress and preventing loss of function. Carbon dioxide can be used to prevent adhesions during abdominal surgery, and to protect the lungs during mechanical ventilation.
Enough carbon dioxide is important in preventing an exaggerated and maladaptive stress response. A deficiency of carbon dioxide (such as can be produced by hyperventilation, or by the presence of lactic acid in the blood) decreases cellular energy (as ATP and creatine phosphate) and interferes with the synthesis of proteins (including antibodies) and other cellular materials.
Bicarbonate to the Rescue
For hundreds or even thousands of years, the therapeutic value of carbonated mineral springs has been known.
Baking soda is the wonderful medicine it is because it gives us instant access to more CO2 without exercise and without slowing down our breathing. Either stomach acid or
lemon added to bicarbonate turns baking soda instantly into carbon dioxide.
 I did check i.e. eBay but, IDK, they look fake to me...
I did check i.e. eBay but, IDK, they look fake to me... 





 .
.